A Comparative Analysis of Ceftaroline versus Vancomycin in Managing Complex Skin Infections
Key Takeaways
- Both ceftaroline and vancomycin are effective in managing cSSTIs, with similar cure rates observed for both antibiotics.
- Patients treated with vancomycin tend to have shorter hospital stays compared to those treated with ceftaroline, which benefits healthcare system efficiency.
- Despite patients receiving ceftaroline often presenting with more severe conditions, the safety profile and secondary health outcomes of both antibiotics are comparable.
Did You Know?
Understanding Complex Skin and Soft Tissue Infections
Complex skin and soft tissue infections (cSSTIs) often arise from common pathogens, but cases involving resistant bacteria like Methicillin-resistant Staphylococcus aureus (MRSA) present significant treatment challenges. These infections demand effective therapeutic responses due to their potential severity and complications.
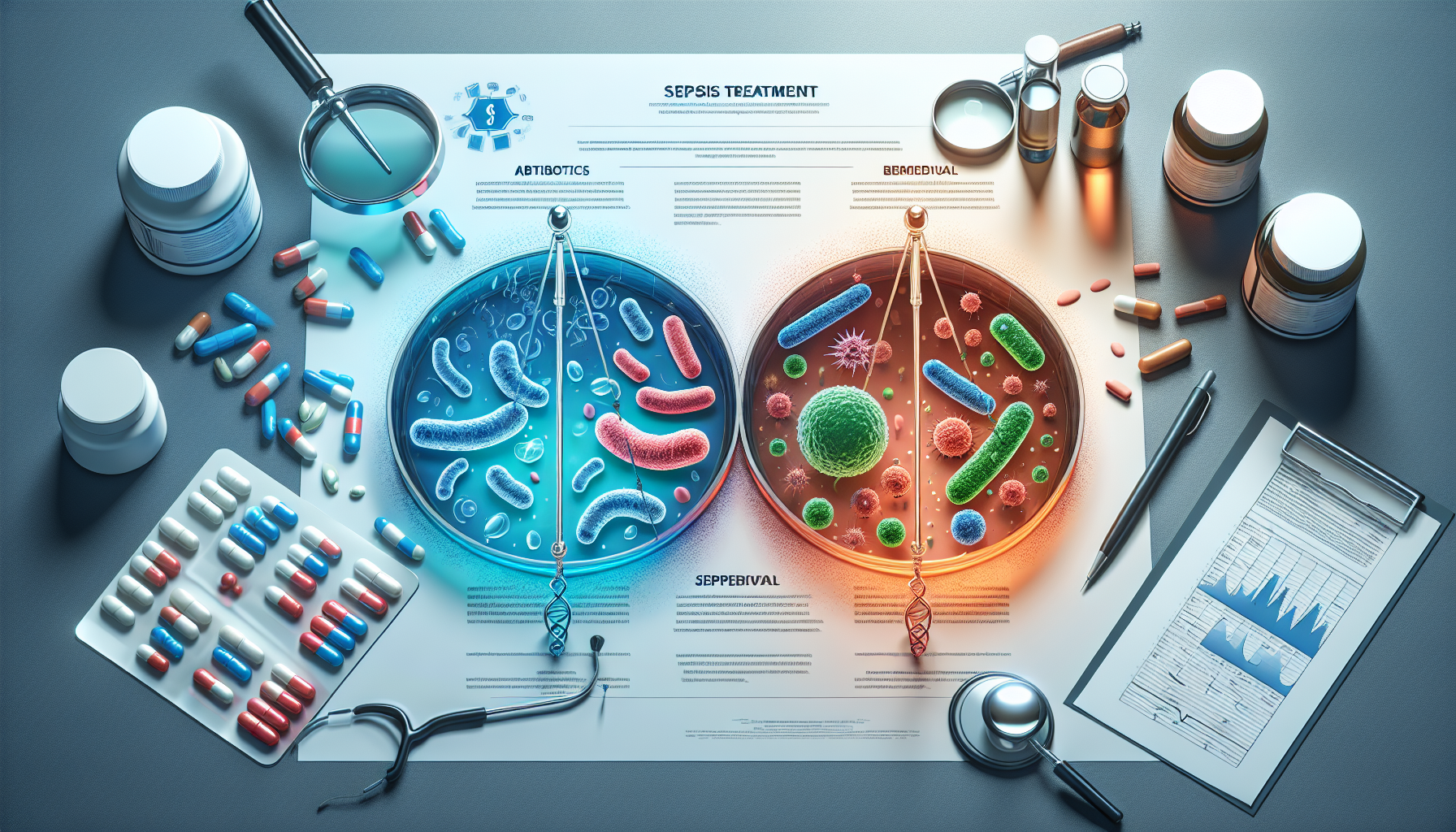
Treatment Options: Ceftaroline vs. Vancomycin
In the clinical battleground against cSSTIs, two antibiotics, ceftaroline and vancomycin, are commonly employed. Recent studies have compared their efficacy, providing insights that are crucial for frontline healthcare providers. Each drug comes with its strengths and considerations, influencing hospital protocols and treatment outcomes.
Study Insights on Efficacy and Hospital Stay
Research analyzing the outcomes of treatment with ceftaroline versus vancomycin shows that both drugs are effective in managing infections. However, interestingly, patients treated with vancomycin tend to have shorter hospital stays, which is beneficial for healthcare system efficiency and reduces patient inconvenience.
Examination of Disease Severity and Cure Rates
When comparing the severity of infections treated, patients receiving ceftaroline often present with slightly more severe conditions. Despite this, the cure rates observed in the study were quite similar between the two groups, indicating that ceftaroline is capable of managing even the more severe infections effectively.
Secondary Health Outcomes Explored
The research also looked at aspects such as the recurrence of infections, safety in terms of kidney health, and the timing for switching from intravenous to oral antibiotics. No significant differences were found in these areas, underscoring the comparable safety profile and effectiveness of both antibiotics.
Demographic and Health Parameters in Study Participants
The study included a diverse group of adults undergoing treatment for cSSTIs. Parameters such as age, body mass index, and various health scores related to physiology and organ failure were similar across both groups treated with ceftaroline and vancomycin, indicating balanced study conditions.
Interim Analysis and Study Population
An interim analysis involving over a hundred participants who received at least 48 hours of treatment sheds light on initial findings. This analysis is vital as it includes a range of adult patients, providing a broad basis for evaluating treatment effectiveness and safety.
Future Directions in Treatment Research
While current findings are promising, ongoing research is essential. A comprehensive analysis of the full sample will provide deeper insights into optimizing treatment strategies for cSSTIs, especially those caused by resistant pathogens such as MRSA.
Clinical Implications and Recommendations
The outcomes of this comparative study are significant for clinical practice, offering evidence-based guidance for choosing between ceftaroline and vancomycin. Healthcare providers are better equipped to tailor treatment plans to individual patient needs, potentially enhancing recovery rates and overall health outcomes.
Conclusion
This investigation highlights the importance of continuous research in improving the management of complicated infections. The comparative efficacy and safety of ceftaroline and vancomycin provide valuable information for clinicians dealing with complex cSSTI cases.