Acetaminophen Shows No Survival Benefit in Sepsis Patients
Key Takeaways
- Acetaminophen did not improve survival or reduce organ support need in sepsis.
- The drug showed safety with no significant adverse events.
- Future studies may explore biomarkers for selecting patients who could benefit.
Did You Know?
Introduction to the ASTER Trial
The ASTER trial, a phase IIb study, explored the effects of intravenous acetaminophen on critically ill patients with sepsis. Researchers aimed to see if the drug could improve survival rates or reduce the need for organ support. The trial's results were shared at the American Thoracic Society annual meeting and published in JAMA.
Study Findings
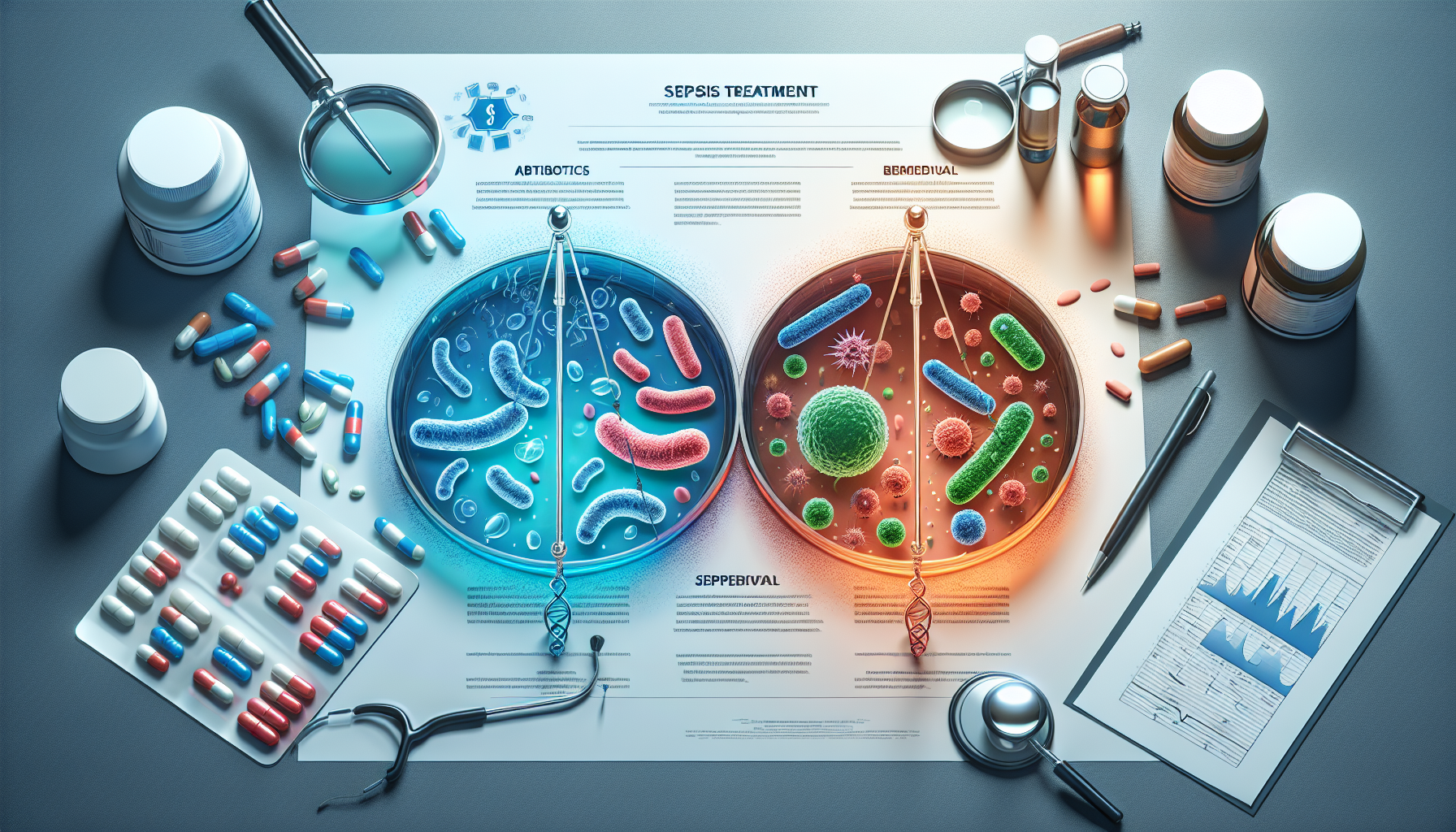
The study found no significant improvement in survival or reduction in organ support needs among those receiving acetaminophen compared to a placebo. Patients in the acetaminophen group had a mean of 20.2 days alive and free from organ support, similar to the 19.6 days in the placebo group.
All-cause mortality at 28 days was 18% for acetaminophen-treated patients compared to 23% for those on placebo. At 90 days, mortality figures were 26% and 32%, respectively. These differences were not statistically significant.
Secondary Outcomes and Potential Biomarkers
Though the primary outcomes were negative, some secondary outcomes showed promise. Only 2.2% of patients in the acetaminophen group developed acute respiratory distress syndrome (ARDS), compared to 8.5% in the placebo group. Improvements in the Sequential Organ Failure Assessment (SOFA) scores were also noted in the acetaminophen group.
Researchers conducted exploratory analyses to see if plasma cell-free hemoglobin levels could identify patients who might benefit from acetaminophen. However, no significant differences in 28-day mortality were observed based on hemoglobin levels.
Clinical Implications
Despite the negative results, the study confirmed the safety of acetaminophen in sepsis patients. There were no differences in hepatic injury, systemic hypotension, or other adverse events between the acetaminophen and placebo groups. Hence, acetaminophen remains a safe option for managing fever and pain in these patients.
Expert Opinions
Robert Dickson, MD, emphasized the importance of the findings, noting that most drug trials in sepsis have been negative. He expressed interest in further studies focusing on septic patients with elevated cell-free hemoglobin levels.
Eligibility Criteria for Participants
Participants had to be critically ill, requiring vasopressors, rehydration, or assisted ventilation. They had to be admitted to the ICU within 36 hours of presenting to the emergency department or acute care.
Demographics and Enrollment
The study included 447 adult patients, with a mean age of 64 years. Most participants were white, and about half were female. Pneumonia was the most common underlying infection.
Treatment Protocol
Patients were randomized to receive either 1g of IV acetaminophen every 6 hours or a placebo. The acetaminophen group received around 12 doses, while the placebo group received approximately 13 doses over 5 days.
Conclusion
While acetaminophen did not show a survival benefit in sepsis patients, it was found to be safe. Future research may explore specific biomarkers to identify patients who might benefit from the treatment.