FDA Approves At-Home HPV Test to Boost Cervical Cancer Screening
Key Takeaways
- FDA approves at-home HPV test, increasing accessibility for cervical cancer screening.
- Home testing can reduce healthcare disparities, benefiting high-risk populations.
- Rapid, accurate results improve early detection and treatment of cervical cancer.
Did You Know?
Introduction to the New Self-Collection HPV Test
The U.S. Food and Drug Administration (FDA) has recently given the green light to a pioneering human papillomavirus (HPV) self-collection solution. This groundbreaking approval marks a significant step toward improving cervical cancer screening accessibility for women nationwide.
How the Self-Collection HPV Test Works
With this innovative solution, women can now collect their own vaginal samples in the privacy of their homes. These self-collected samples are then sent to a lab for analysis using Roche’s cobas® molecular HPV test. If the test results are positive for HPV, individuals can follow up with their healthcare providers for further evaluation and care.
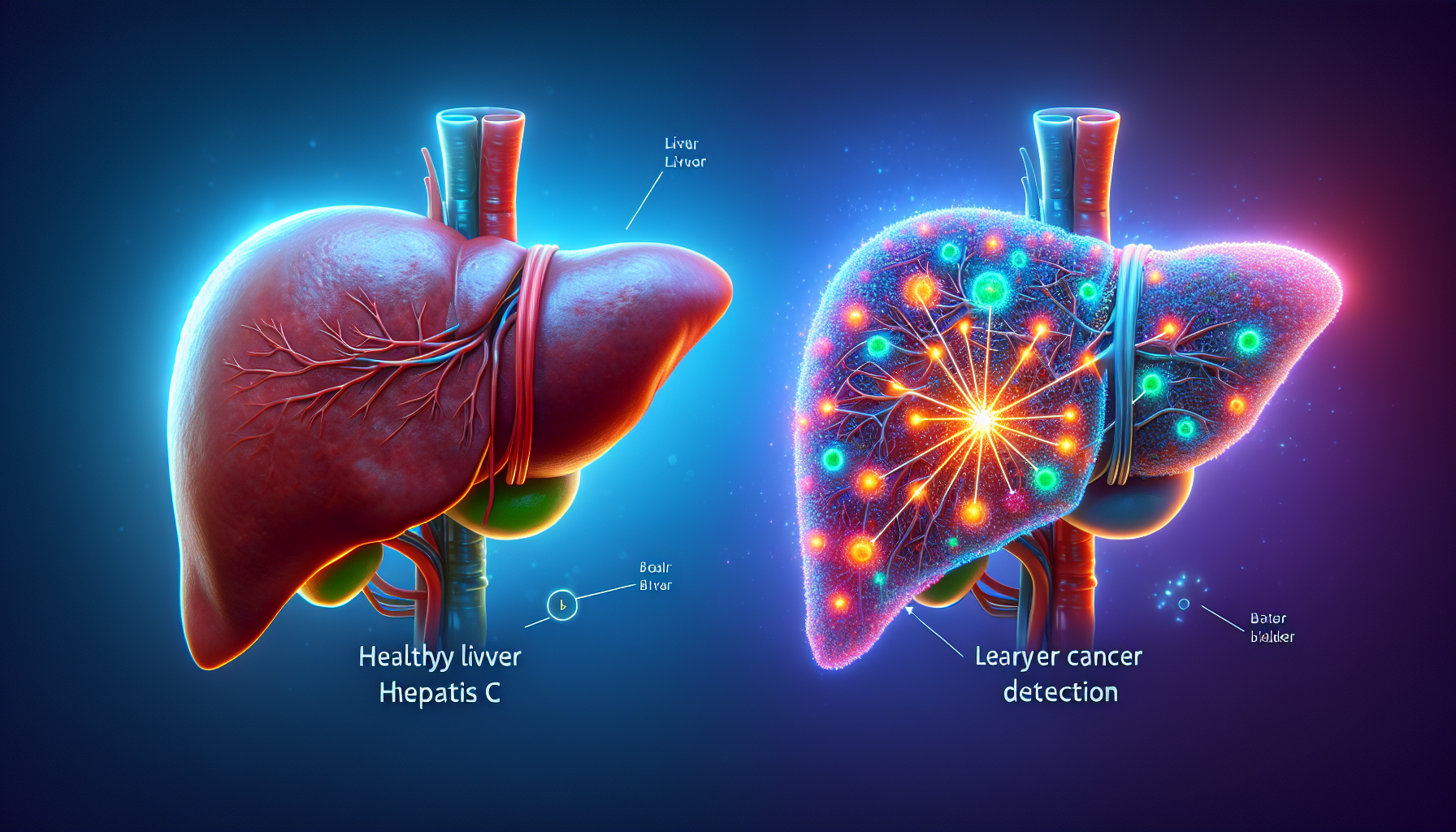
The Importance of HPV Testing and Early Detection
HPV is a major risk factor for cervical cancer, and early detection through regular screening is crucial in preventing the progression of the disease. Traditional screening methods like Pap smears identify abnormal cervical cells, while the cobas® HPV test can detect 14 types of high-risk HPV that are linked to cervical cancer.
Advancements in Screening Technology
The cobas® HPV test works with several of Roche’s automated systems, offering rapid and accurate results. For instance, the cobas® 4800 system can deliver up to 96 results in approximately three hours, while the cobas® 6800 and 8800 systems can handle larger volumes, producing 384 to 1056 results within an 8-hour shift.
Supporting Underserved Populations
The approval of this self-collection solution is particularly significant for underserved populations. Studies have shown that Black, Hispanic, and American Indian women have higher rates of cervical cancer. The highest mortality rate is seen among Black women. This new screening method provides a more accessible option for these communities, helping to reduce healthcare disparities.
Clinical Trials and Validations
The clinical benefits of the self-collection solution were validated in the IMPACT trial, which included 35,263 participants from diverse backgrounds. Results from this trial demonstrated the effectiveness of the cobas® HPV test in identifying high-risk HPV infections, providing a reliable method for early detection.
Reducing Barriers with Home Testing
Offering the self-collection solution aims to remove barriers to cervical cancer screening, such as the discomfort or inconvenience associated with going to a clinic. This accessibility may encourage more women to undergo regular screening, leading to earlier detection and better outcomes.
Collaborations and Initiatives
Roche collaborated with the National Cancer Institute for the Cervical Cancer “Last Mile” Initiative, which focuses on addressing screening disparities. This partnership has been instrumental in paving the regulatory path for the FDA's recent approval.
Understanding the Risks and Benefits
The IMPACT trial found that the cumulative risk for cervical intraepithelial neoplasia grade 3 or higher was significantly higher in patients who tested positive for HPV 16 compared to those who were HPV-negative. This illustrates the importance of effective screening for early intervention and treatment.
Conclusion and Future Implications
The FDA’s approval of the HPV self-collection solution is a monumental advancement in the fight against cervical cancer. With improved accessibility, it has the potential to significantly increase screening rates, particularly in underserved communities, bringing us closer to the goal of eliminating cervical cancer by 2030.