How Primary Care Providers Can Enhance Rhinitis Treatment with Specific IgE Testing
Key Takeaways
- Accurate diagnosis of rhinitis improves patient care.
- Specific IgE testing helps distinguish between AR and NAR.
- Proper diagnosis can reduce unnecessary medication use.
Did You Know?
Understanding Rhinitis: A Common Condition
Rhinitis, characterized by symptoms such as coughing, sneezing, a runny or congested nose, and itchy eyes, nose, throat, and ears, is a prevalent condition affecting many. For primary care providers (PCPs), distinguishing between allergic rhinitis (AR) and nonallergic rhinitis (NAR) is crucial due to their overlapping symptoms.
Accurate diagnosis is crucial for effective treatment. Symptoms can range from mild irritation to severe discomfort, affecting a patient's quality of life significantly. Without proper diagnosis, symptom management may be suboptimal, potentially leading to sleep deprivation and mental health issues.
The Importance of Accurate Diagnosis
Accurate diagnosis not only helps in better symptom management but also reduces unnecessary medication costs and exposure to allergens. Studies have shown that nearly two-thirds of patients prescribed antihistamines for suspected allergies actually have nonallergic symptoms.
The economic impact of rhinitis is also noteworthy, with billions of dollars lost annually due to reduced productivity and missed work or school. Thus, it is essential for PCPs to use diagnostic tools like specific IgE testing to differentiate between AR and NAR.
Introducing Specific IgE Testing
Specific IgE testing measures the levels of allergen-specific IgE antibodies in a patient's blood. This provides valuable information about allergic sensitizations, allowing PCPs to rule in or out AR efficiently. This test can be conducted in primary care settings, offering a practical solution to the current lack of diagnostic testing.
Using this method, PCPs can develop accurate, patient-specific treatment plans, mitigating unnecessary medication use and improving overall patient outcomes.
Guidelines and Best Practices
According to guidelines from The Journal of Allergy and Clinical Immunology, confirming the diagnosis of AR through aeroallergen skin prick testing or serological testing is recommended. However, many PCPs still manage rhinitis without these diagnostic tools, potentially affecting treatment outcomes.
Embracing specific IgE testing can enhance the accuracy of diagnosis and subsequent management plans. By determining the exact allergens causing symptoms, PCPs can better advise on avoidance strategies and appropriate medication.
Implementing Specific IgE Testing
Implementing specific IgE testing in primary care is straightforward. The process involves a clinical evaluation followed by ordering the specific IgE blood test. The blood sample is analyzed for sensitization to whole allergens and components, and the results are interpreted by the PCP.
If the results indicate nonallergic causes, further evaluation and referrals to specialists can be made. If allergic causes are found, PCPs can implement targeted allergy reduction strategies and appropriate treatments.
Regional Profiles and Comprehensive Care
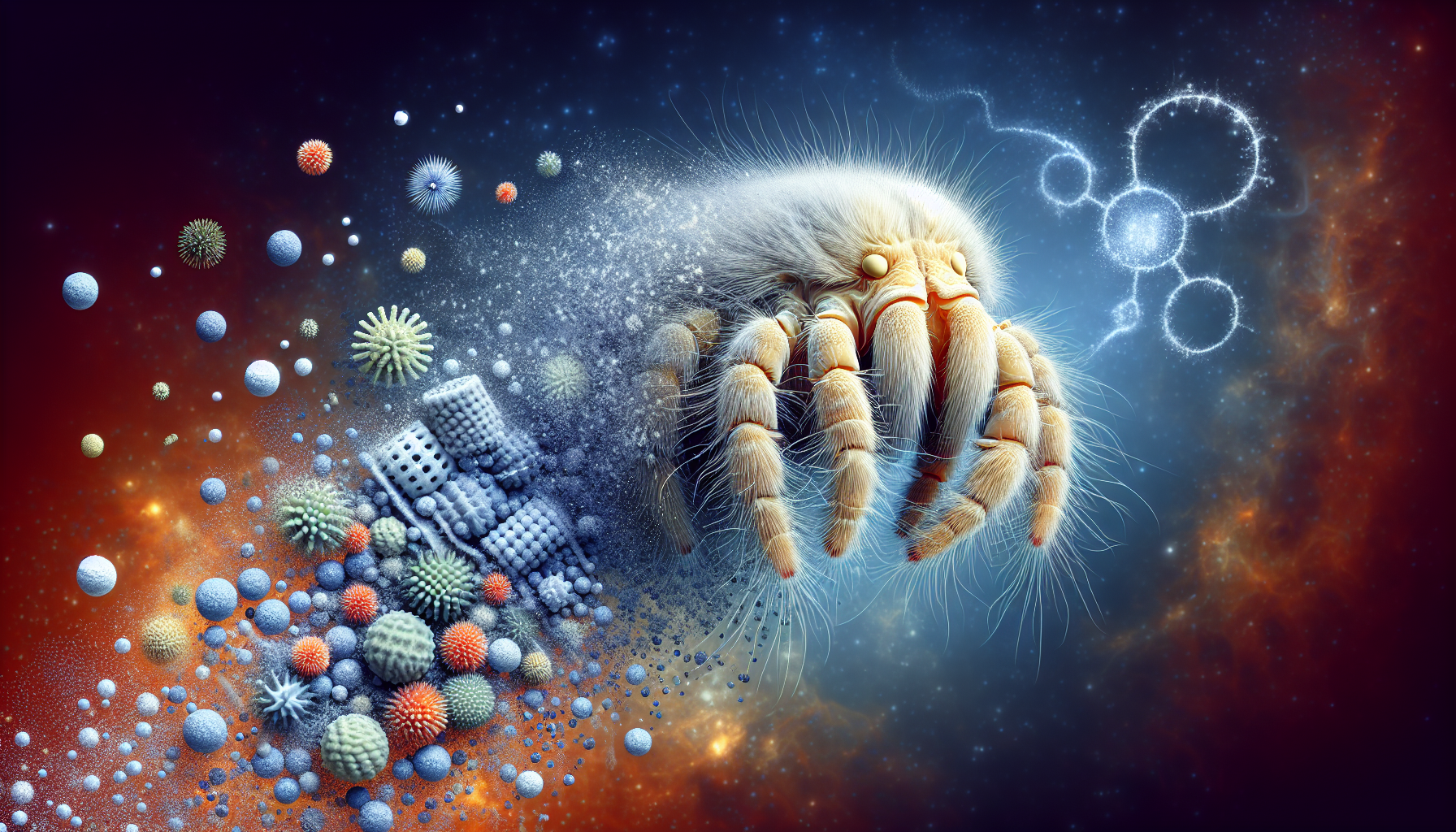
Specific IgE tests can also be used to create regional respiratory profiles, including common local allergens such as dust mites and pet dander. This helps in forming a more comprehensive understanding of the patient's sensitivities and managing their condition more effectively.
These profiles allow for efficient and targeted testing, which is crucial in regions with diverse allergen exposures, enhancing patient care and treatment outcomes.
Better Patient Care and Reduced Misdiagnosis
The integration of specific IgE testing in diagnosing and managing rhinitis can significantly reduce misdiagnosis. Accurate identification of allergenic causes leads to better-targeted interventions, optimizing health outcomes and improving the quality of life for patients.
By replacing the best guess approach with evidence-based practice, PCPs can ensure more effective management strategies, ultimately benefiting public health on a broader scale.
Conclusion
In summary, specific IgE testing is a valuable tool for PCPs in diagnosing and managing rhinitis effectively. By enhancing diagnostic accuracy, PCPs can provide better-targeted treatments, reducing unnecessary medication use and improving patient outcomes.
As respiratory allergies continue to rise, embracing specific IgE testing in primary care settings is essential in providing high-quality, patient-centric care.
Take the Next Step
For PCPs looking to improve their care strategies for rhinitis patients, integrating specific IgE testing offers a clear pathway toward better diagnosis, treatment, and overall health outcomes. Start implementing this test in your practice today to see the positive difference it can make.