Innovative Thrombectomy Devices Enhance Treatment for Pulmonary Embolism
Key Takeaways
- Recent advancements in thrombectomy devices, specifically the AlphaVac F1885 from AngioDynamics and the Hlo PE system from Endovascular Engineering, have shown significant improvements in treating intermediate-risk pulmonary embolism.
- The APEX-AV trial demonstrated that the AlphaVac F1885 system effectively reduces the RV/LV ratio and clot burden with a low incidence of major adverse events, receiving FDA 510(k) clearance for its safety and efficacy.
- The ENGULF trial highlighted the Hlo PE system's innovative approach and ability to significantly reduce thrombus burden and improve cardiac function, suggesting its potential to become a standard tool in PE treatment.
Did You Know?
Introduction to New Thrombectomy Technologies
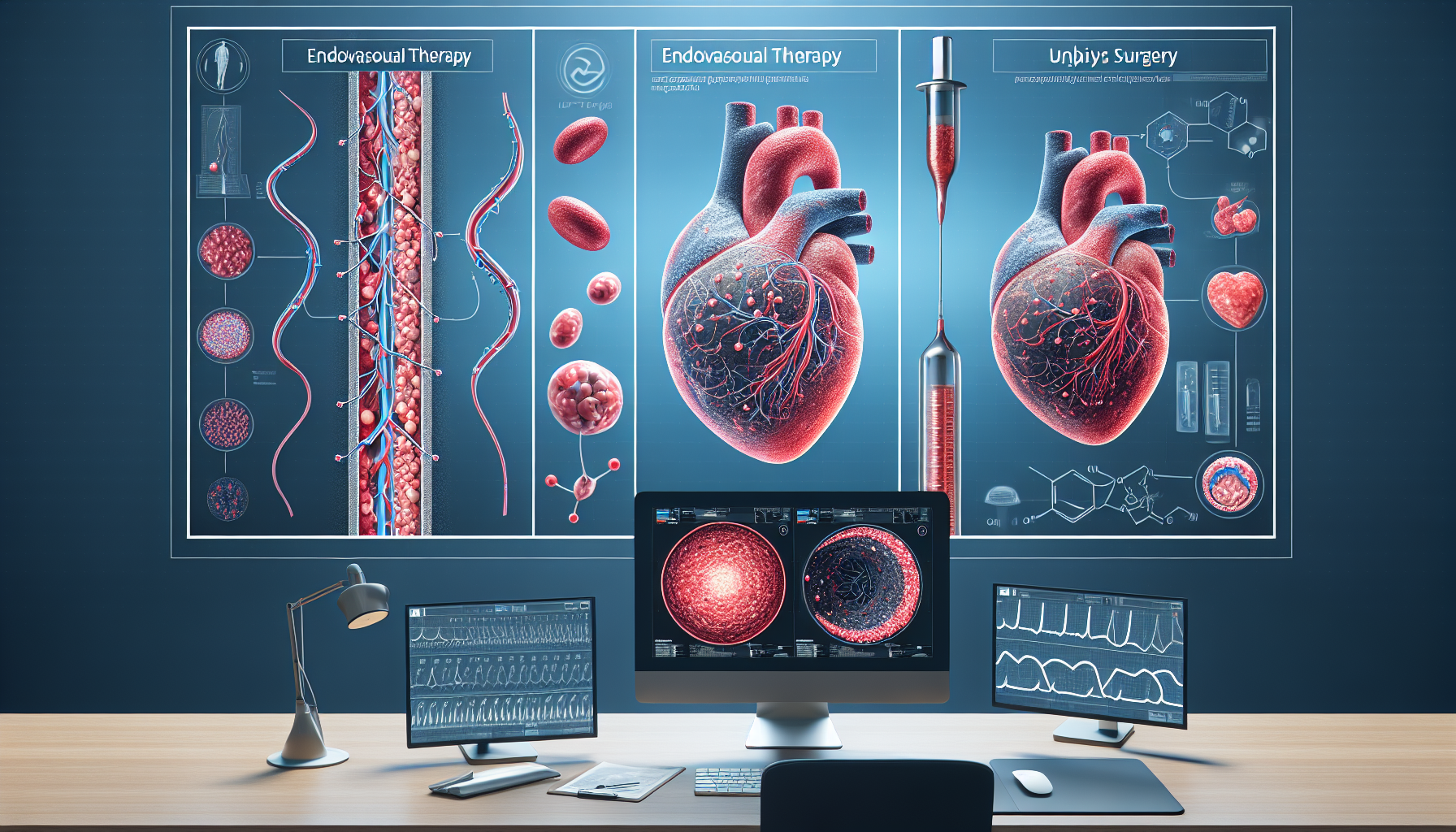
Recent advancements in medical technology have introduced two groundbreaking thrombectomy devices designed to improve the treatment of intermediate-risk pulmonary embolism (PE). These devices, which were highlighted in recent clinical trials, offer new hope for patients suffering from this serious condition. Pulmonary embolism, a blockage in one of the pulmonary arteries in the lungs, can be life-threatening if not treated promptly and effectively.
The APEX-AV Trial Outcomes
The APEX-AV trial, a significant study involving 122 patients, tested the AlphaVac F1885 system by AngioDynamics. This mechanical aspiration thrombectomy system is designed to remove blood clots from the lungs quickly and safely. The trial reported a notable reduction in the right ventricle-to-left ventricle (RV/LV) ratio, a critical measure of cardiac function, which improved by approximately 29.1% post-procedure. Furthermore, the trial demonstrated a low incidence of major adverse events, highlighting the device's safety.
Another key finding from the APEX-AV trial was the reduction in clot burden and pulmonary artery pressure, which are essential indicators of the effectiveness of PE treatment. The device also received FDA 510(k) clearance, affirming its safety and efficacy for clinical use.
ENGULF Trial Innovations
The ENGULF trial introduced the Hlo PE system from Endovascular Engineering, a novel approach to thrombectomy that incorporates a steerable and expandable funnel with an internal spinning agitator to enhance clot breakdown. This trial involved 28 patients and focused on the device's feasibility and safety. Results showed a significant decrease in the RV/LV ratio by 23.2%, indicating substantial improvement in cardiac function after the procedure.
Moreover, the ENGULF trial emphasized the device's ability to significantly reduce thrombus burden in targeted pulmonary arteries, with an 80% reduction observed on angiography. This points to the device's potential to offer a more effective treatment for PE, addressing previous challenges such as incomplete clot removal and potential vascular injury.
Comparative Analysis and Future Directions
Both the APEX-AV and ENGULF trials represent significant strides in the treatment of pulmonary embolism, showcasing devices that not only improve patient outcomes but also maintain high safety profiles. The comparative effectiveness of these devices with existing FDA-approved options suggests that they could soon become standard tools in the fight against PE.
As these devices continue to be evaluated in further studies, their role in clinical practice could expand, providing physicians with more effective tools to combat this dangerous condition. The ongoing research and development in this field are crucial for enhancing patient care and outcomes in pulmonary embolism treatment.