Low-Calorie, Plant-Based Diet Shows Promise for Ulcerative Colitis Management
Key Takeaways
- A low-calorie, plant-based diet improved UC symptoms and inflammation.
- 50% of participants on the diet had a clinical response to therapy.
- Diet could be a valuable tool alongside medication for managing UC.
Did You Know?
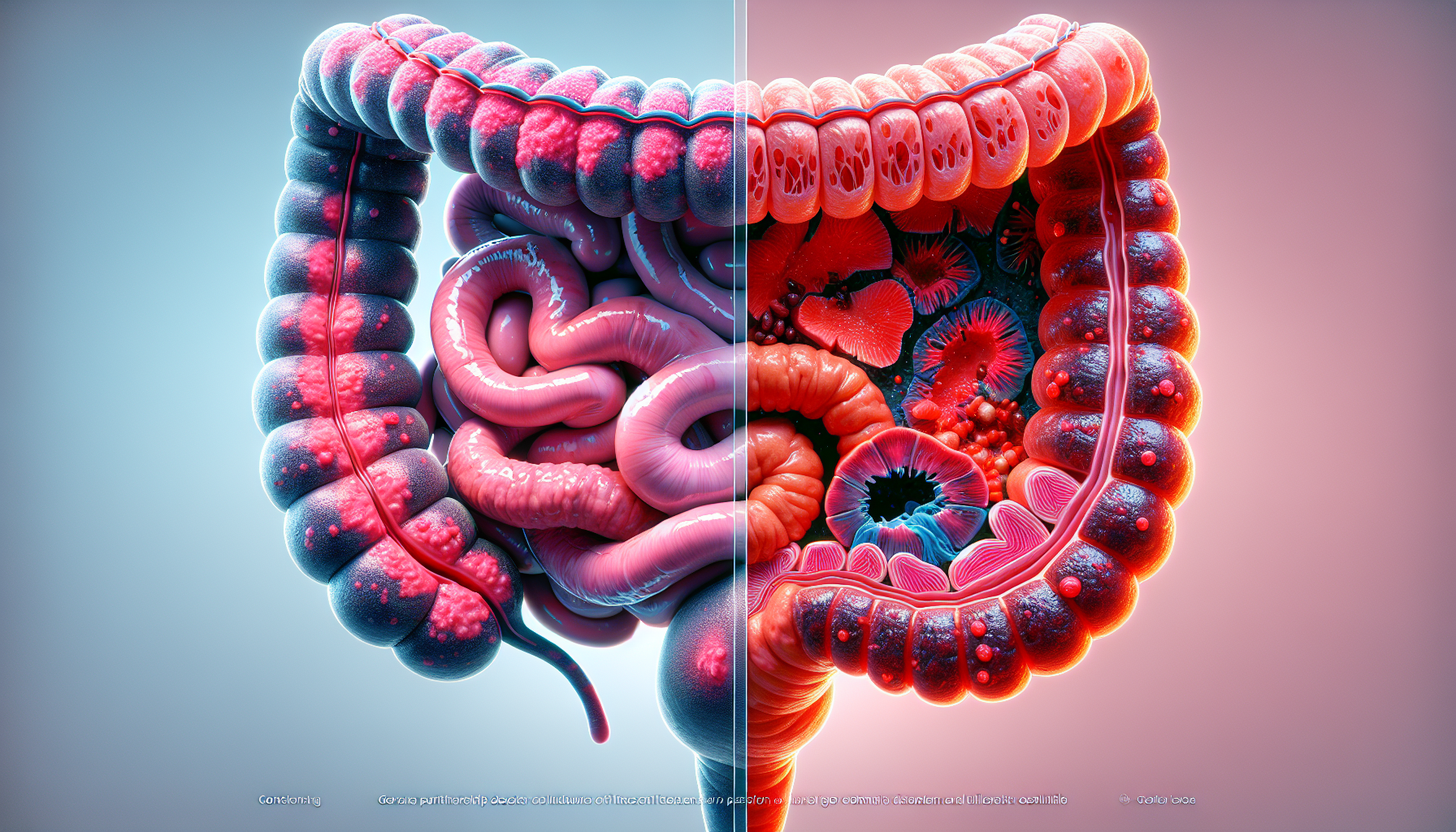
Introduction to Ulcerative Colitis
Ulcerative colitis (UC) is a chronic inflammatory condition affecting the colon. This disease can cause severe symptoms such as abdominal pain, diarrhea, and bleeding. Treatments often involve medications, but recent studies highlight the potential role of diet in managing UC.
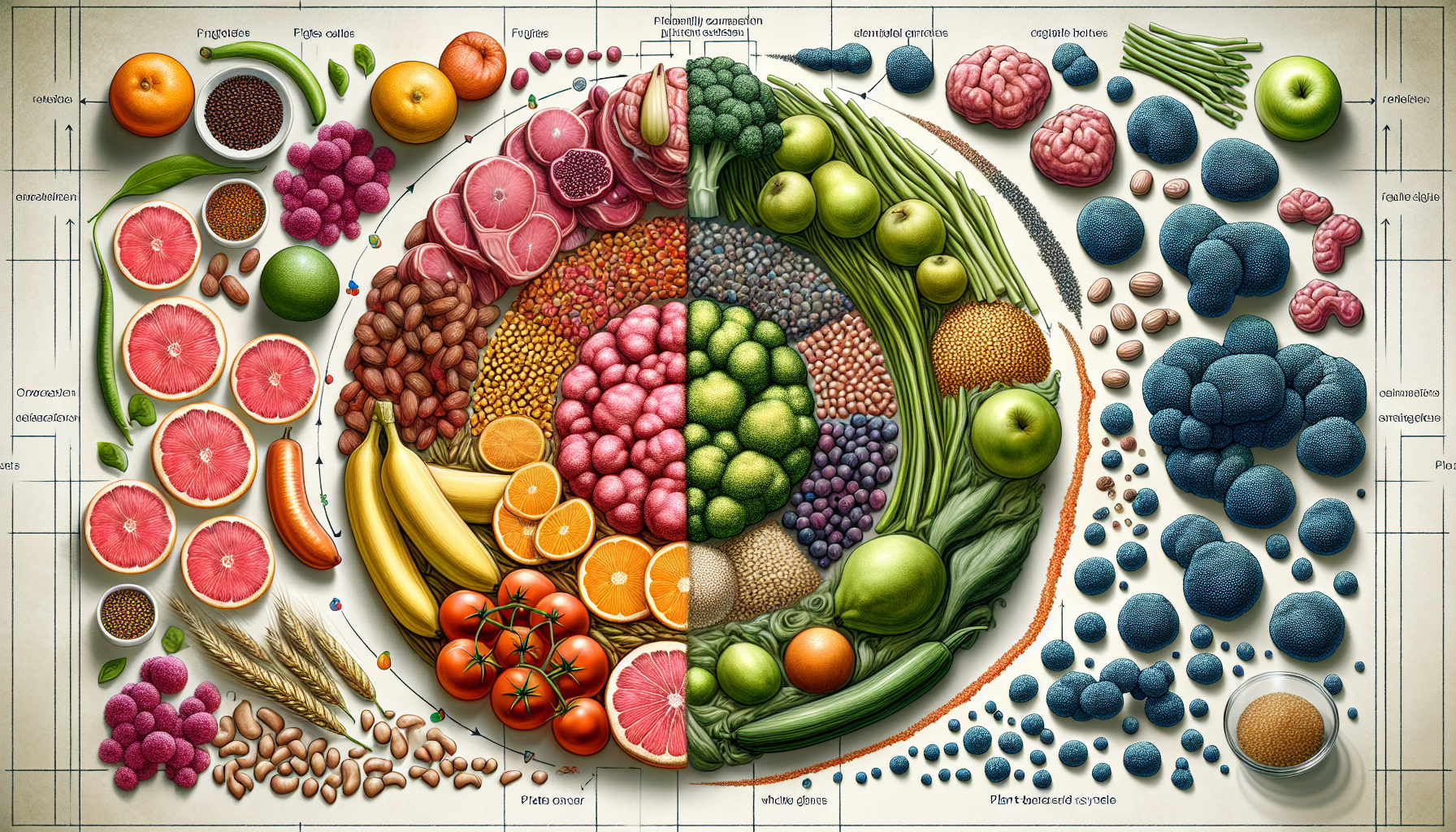
The Role of Diet in UC
Although diet is known to influence inflammation in inflammatory bowel diseases (IBD), there's a lack of clinical trials exploring its impact on UC. Researchers at the University of Miami Miller School of Medicine have conducted a study to examine whether a short-term, low-calorie, plant-based diet can improve inflammation and response to medical therapy in UC patients.
The Study at Digestive Disease Week
During Digestive Disease Week, a team led by Dr. Oriana M. Damas presented findings from a study involving 32 adult patients with moderately to severely active UC. Participants were randomly assigned to follow either a low-calorie, plant-based diet plus their standard medical therapy or a low-residue control diet for 8 weeks.
Dietary Intervention Details
Those on the plant-based diet were provided with commercially available fasting-mimicking diet kits. On the first day, the diet offered approximately 1,090 kcal with a macronutrient split of 10% protein, 56% fat, and 34% carbohydrates. For the next four days, caloric intake was reduced to 725 kcal with 9% protein, 44% fat, and 47% carbohydrates. Adjustments were made based on tolerance and adherence to maintain stable macronutrient percentages.
Exclusion Criteria
Participants who were likely to have issues tolerating a low-calorie intake, such as those with low body mass index (BMI), significant comorbidities, or those over the age of 75, were excluded from the study. This step ensured that the dietary intervention was safe for all participants.
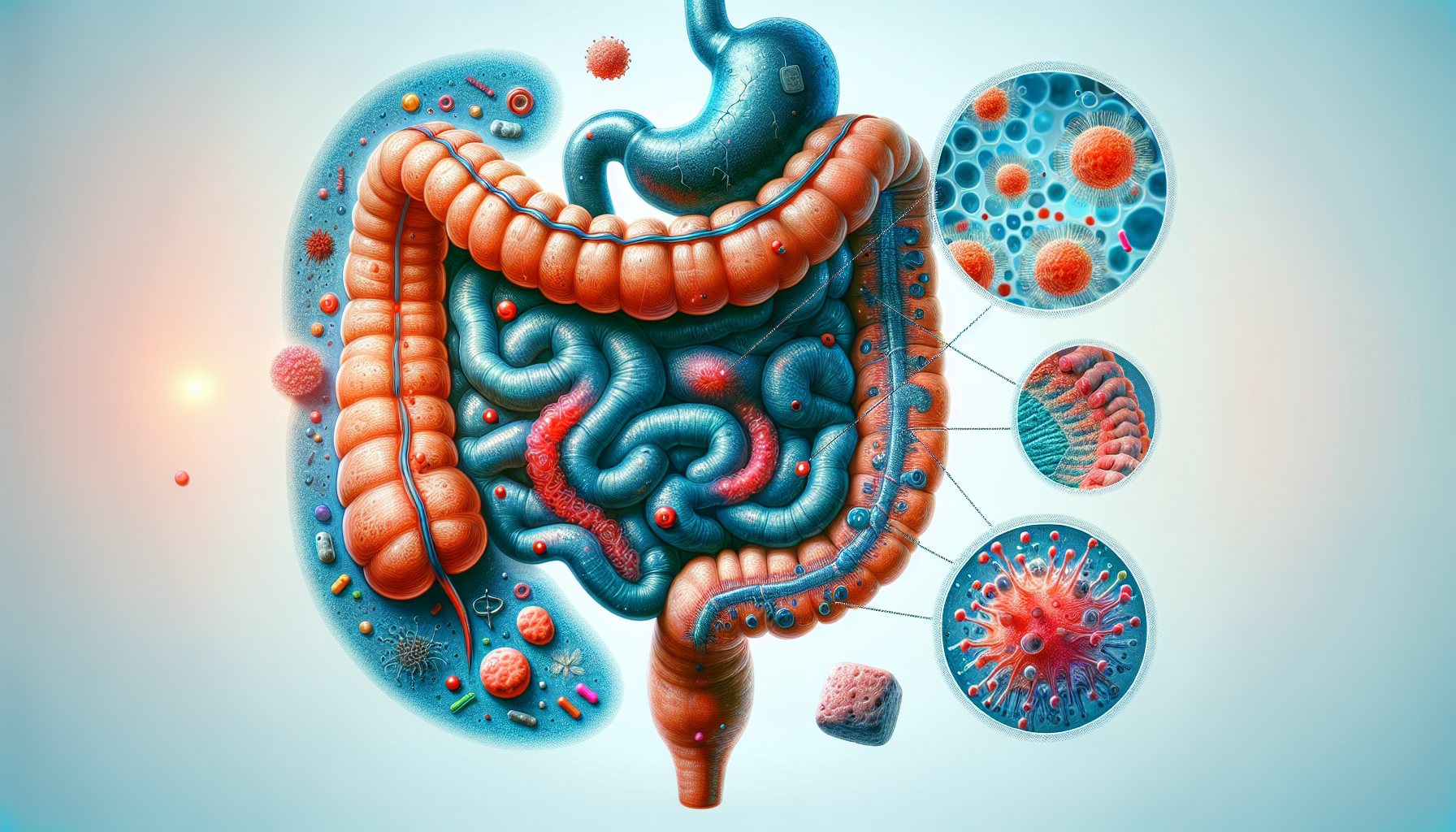
Assessing the Outcomes
The primary outcome measured was the clinical response at week 8 using the Simple Clinical Colitis Activity Index (SCCAI). Secondary outcomes included markers of inflammation such as fecal calprotectin and serum amyloid A protein levels. Blood and stool samples were collected and analyzed throughout the study.
Results of the Study
The study found that participants on the plant-based diet showed significant improvement in all components of the SCCAI, including well-being, urgency, and presence of blood in the stool, compared to the control diet group. At week 8, 50% of those on the plant-based diet experienced a clinical response to therapy, compared to 30.7% in the control group. The mean reduction in SCCAI scores was higher in the plant-based diet group than in the control group (4.4 vs. 1.61).
Inflammatory Markers
Although the improvement in fecal calprotectin did not reach statistical significance, there was a notable enhancement in serum amyloid A protein levels, which is a sensitive marker of inflammation in the blood.
Clinical Implications
Dr. Damas highlighted the potential of diet as an adjunct to medical therapy in managing UC. Short intervals of a low-calorie, plant-based diet could provide an additional tool to help reduce inflammation and improve patients' response to medications.
Future Directions
Further research is needed to confirm these findings and explore the long-term benefits of dietary interventions in UC management. However, this study opens the door for considering diet as a significant factor in treating UC.