Persistent Mucus in Severe Asthma: What Biologics Can't Clear
Key Takeaways
- Biologics do not completely eliminate mucus plugs in severe asthma.
- Residual mucus is linked to worse asthma control even with biologics.
- Advanced imaging and tailored treatments are essential for better management.
Did You Know?
Understanding Severe Asthma and Mucus Plugging
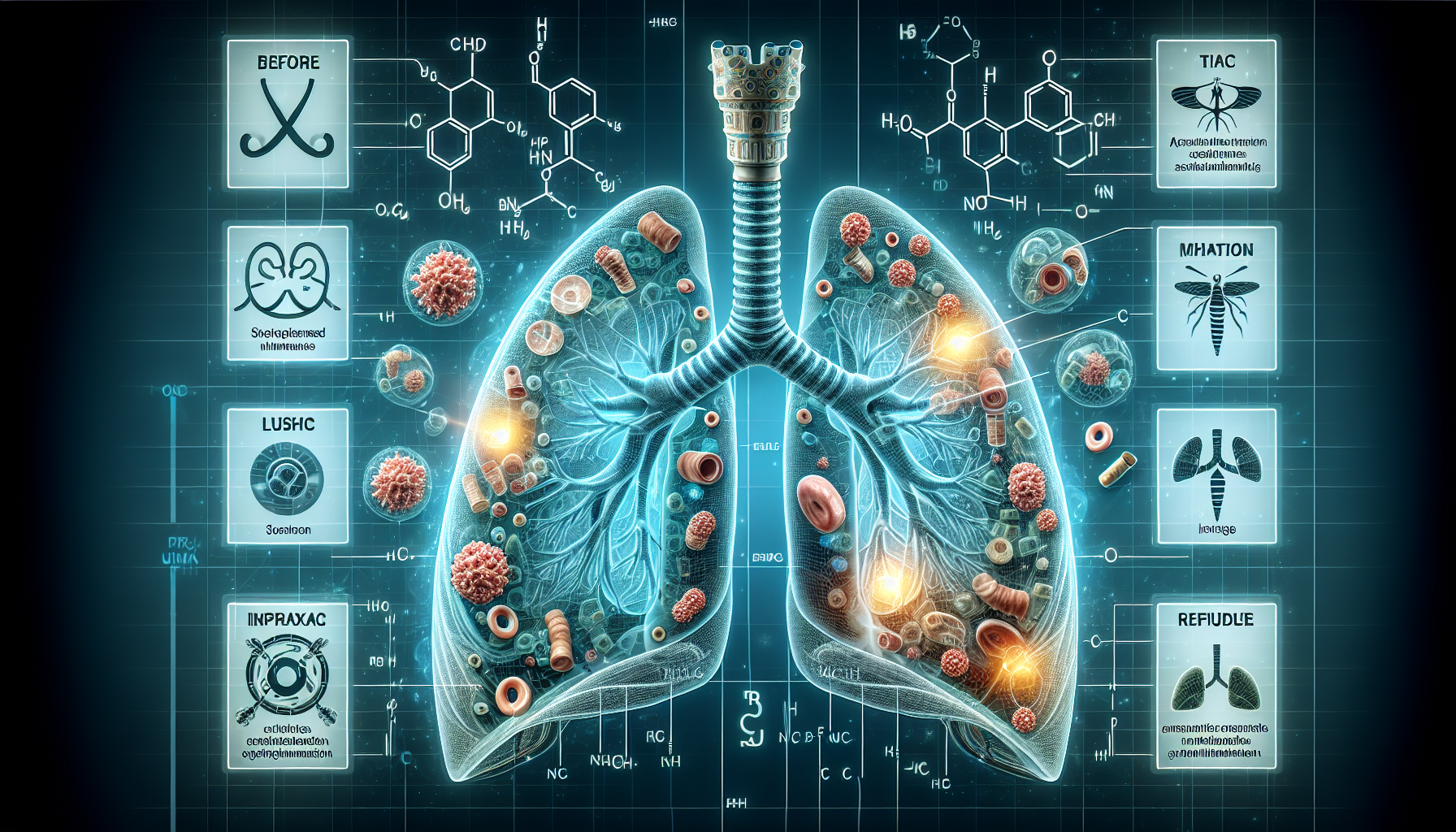
Severe asthma is a condition where patients experience significant difficulty in breathing due to inflammation and narrowing of the airways. One of the critical contributors to this condition is the presence of mucus plugs, which can block the air passages and make it harder for patients to breathe.
Recent research presented at the American Thoracic Society International Conference has highlighted an important finding: patients with severe asthma often have residual mucus plugging even when they are treated with advanced biologic therapies.
What Are Biologics?
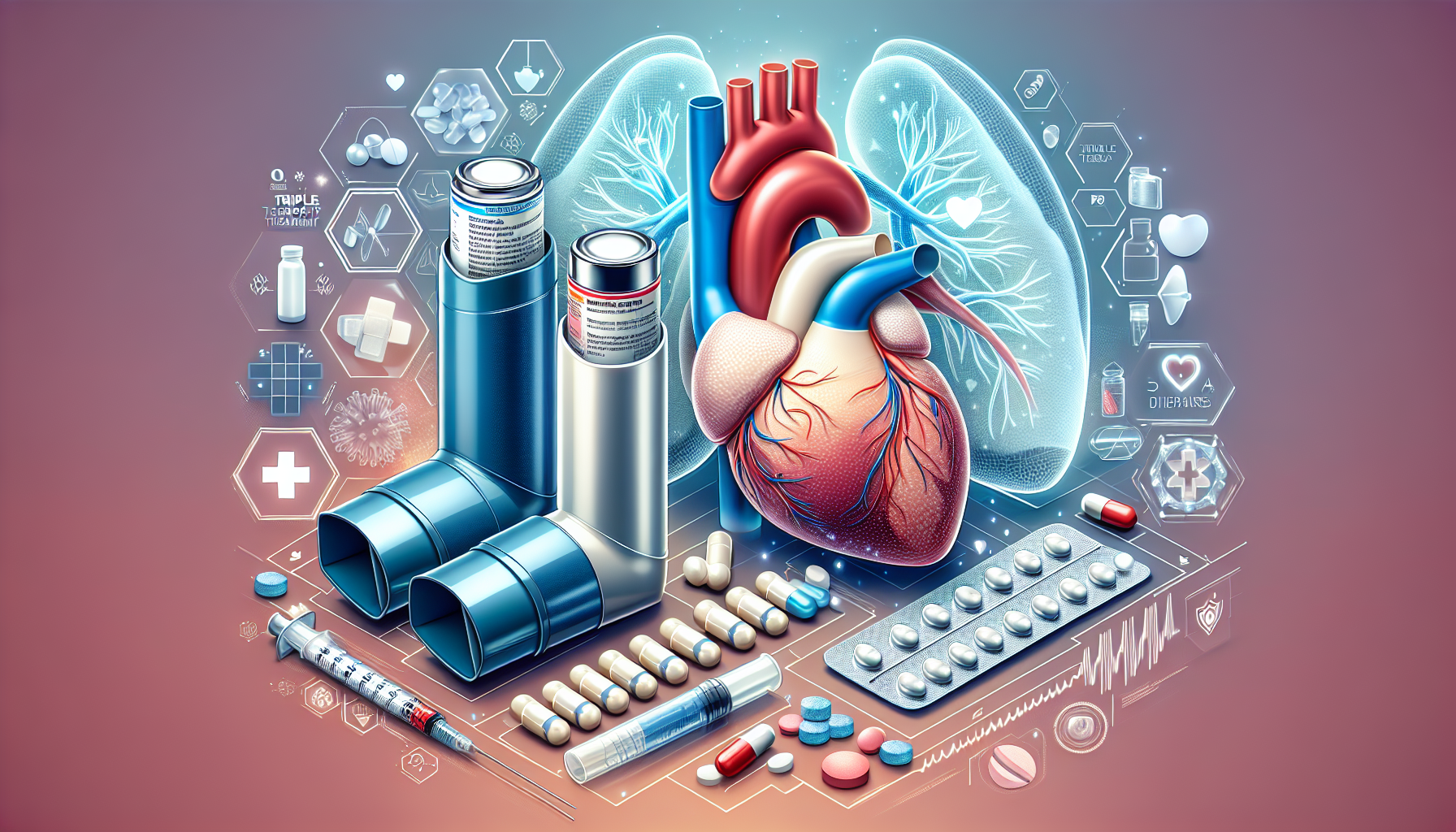
Biologics are a type of treatment that uses monoclonal antibodies to target specific pathways involved in the inflammation process of asthma. These therapies are designed to reduce the number of inflammatory cells like eosinophils in the airways, which are often elevated in severe asthma patients.
Examples of biologics include dupilumab, benralizumab, mepolizumab, and reslizumab. These treatments have revolutionized the management of severe asthma by significantly reducing the disease burden and improving patients' quality of life.
The Study's Findings
The study involved 71 adults with severe asthma who had been on inhaled corticosteroids and, in some cases, systemic steroids. Among them, 36 patients were also receiving biologic treatments. Researchers performed chest CT scans to assess the presence and extent of mucus plugging in these patients.
Results showed that 69% of patients who were not on biologics and 44% of those who were on biologics still had residual mucus plugging. While biologics had some effect on reducing mucus scores, they did not completely eliminate the mucus plugs.
Impact on Asthma Control
The study further noted that even among patients on biologics, those with higher mucus scores had worse asthma control and more severe airflow obstruction. Asthma control was measured using a standardized questionnaire, and airflow obstruction was assessed through lung function tests.
Interestingly, the presence of residual mucus did not correlate with blood eosinophil levels or other common markers of inflammation. This suggests that mucus plugging in severe asthma might involve different mechanisms that are not directly addressed by current biologic therapies.
Implications for Treatment
The findings from this study underscore the importance of assessing mucus plugging in patients with severe asthma. Physicians are encouraged to use advanced imaging techniques like CT scans to evaluate the extent of mucus in their patients' airways.
This assessment can help tailor treatment strategies more effectively. In some cases, additional therapies beyond biologics might be necessary to manage persistent mucus plugging and achieve better asthma control.
Future Research Directions
Ongoing research is focusing on understanding the nature of mucus in severe asthma and exploring new imaging techniques like magnetic resonance and CT imaging. These advanced imaging methods can provide more detailed insights into mucus composition and its impact on lung function.
Researchers are also investigating other potential therapies that could target mucus more effectively, offering hope for patients who do not respond adequately to current biologic treatments.
Conclusion
Although biologic therapies have significantly improved the management of severe asthma, they may not completely clear mucus plugs in all patients. Regular monitoring and tailored treatment approaches are essential to address this issue and improve asthma control and patient outcomes.
Call to Action
Physicians should consider incorporating mucus assessment in their clinical practice for patients with severe asthma and explore a combination of therapies to address persistent mucus plugging.
Research in this area is crucial to developing better treatment strategies and improving the lives of those affected by severe asthma.