Potential Vaccine for Eczema in Children Offers Hope for Effective Treatment
Key Takeaways
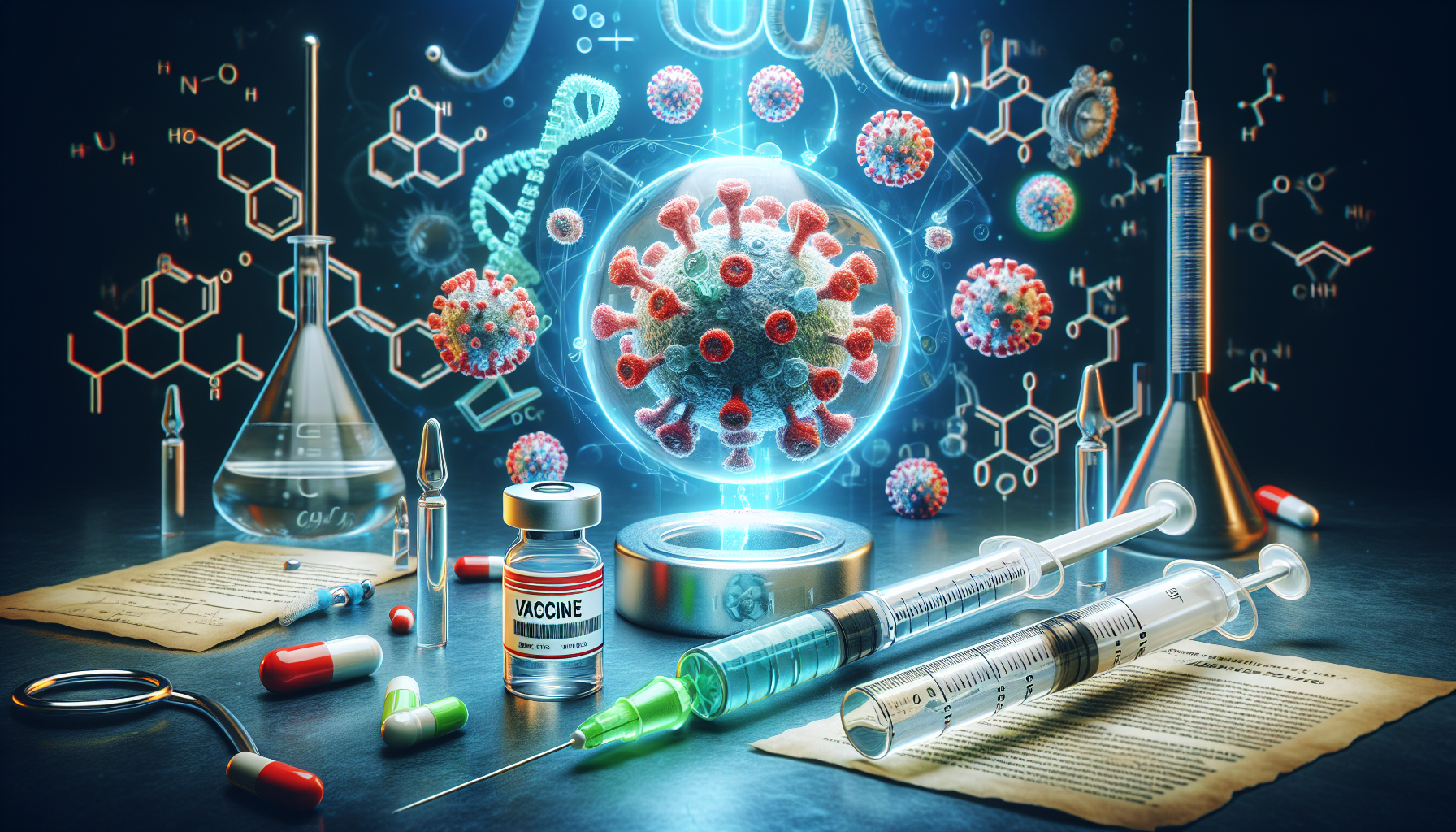
- Recent research aims to develop a specialized vaccine for children with recurrent eczema flare-ups due to bacterial infections.
- The study highlights the suppression of specific T cells in children with infected eczema flare-ups.
- Further research is required to confirm findings across different age groups and ethnicities.
Did You Know?
Understanding the Link Between Eczema and Bacteria
Recent studies have shed light on the relationship between eczema and the bacterium Staphylococcus aureus (S. aureus), suggesting the possibility of developing a specialized vaccine for children who experience recurring flare-ups due to bacterial infection. Research conducted at Trinity College Dublin focused on identifying immune response mechanisms that could be targets for such a vaccine.
Eczema, also known as atopic dermatitis, is a condition that causes dry, itchy skin. In some cases, bacterial infections cause the skin to weep and may lead to severe and potentially life-threatening infections like sepsis. Understanding the immune responses in children with eczema can pave the way for more effective treatments.
Insights from Recent Research
The research led by Julianne Clowry, a dermatologist and visiting research fellow, emphasized the need for better management and prevention strategies for infected eczema flare-ups in children. Current treatments often provide only temporary relief, and there is a growing issue of antimicrobial resistance.
The study evaluated the immune responses of 93 children, aged 0 to 16, divided into three groups: those with atopic dermatitis and S. aureus infection, those with atopic dermatitis but no infection, and a healthy control group. This comparison highlighted variations in certain immune cells called 'T cells' among these groups, offering new insights into the immune profiles linked with S. aureus skin infections in eczema patients.
Key Findings and Implications
One of the crucial findings was a significant variation in the proportions of T cells and other biomarkers among the groups. These variations were linked to how children's immune systems respond to S. aureus infections, with suppressed T cell types playing a crucial role in managing infected eczema flare-ups.
According to the study's senior author, Rachel McLoughlin, the research identified an overall immune suppression pattern associated with infected eczema flares. This suppression affects specific T cells needed for an effective immune response, highlighting potential targets for new treatments.
Future Directions
While the findings are promising, further research is needed to verify whether these immune response patterns are consistent across different age groups and among more ethnically diverse populations. Expanding the scope of this research will help confirm the findings and support the development of targeted treatments for eczema flare-ups.
McLoughlin noted that a deeper understanding of the immune responses to S. aureus in individuals with atopic dermatitis could revolutionize eczema therapy. This could lead to new, more effective management strategies for the condition, offering hope for those who experience recurrent, infected flare-ups.
Conclusion
In summary, the study provides a hopeful outlook for children suffering from recurrent eczema flares caused by bacterial infection. By identifying specific immune response mechanisms, researchers have laid the groundwork for potentially transformative treatments. These promising findings bring us closer to developing a vaccine tailored for children with atopic dermatitis, aiming to provide longer-lasting and more effective relief.