Revolutionizing Diabetes Treatment: Exploring New Subtypes for Tailored Therapies
Key Takeaways
- New diabetes subtypes are being recognized for more personalized treatment.
- Genomic data is crucial for tailoring diabetes therapies.
- AI and wearable devices are enhancing diabetes management.
Did You Know?
The Growing Complexity of Diabetes Treatment
As the methods for treating diabetes expand, it's becoming clear that the disease itself needs a deeper understanding. Researchers now believe that diabetes has more than just the two traditional 'types’ — Type 1 and Type 2. Specialists argue that recognizing these subtypes could lead to more personalized treatments for patients.
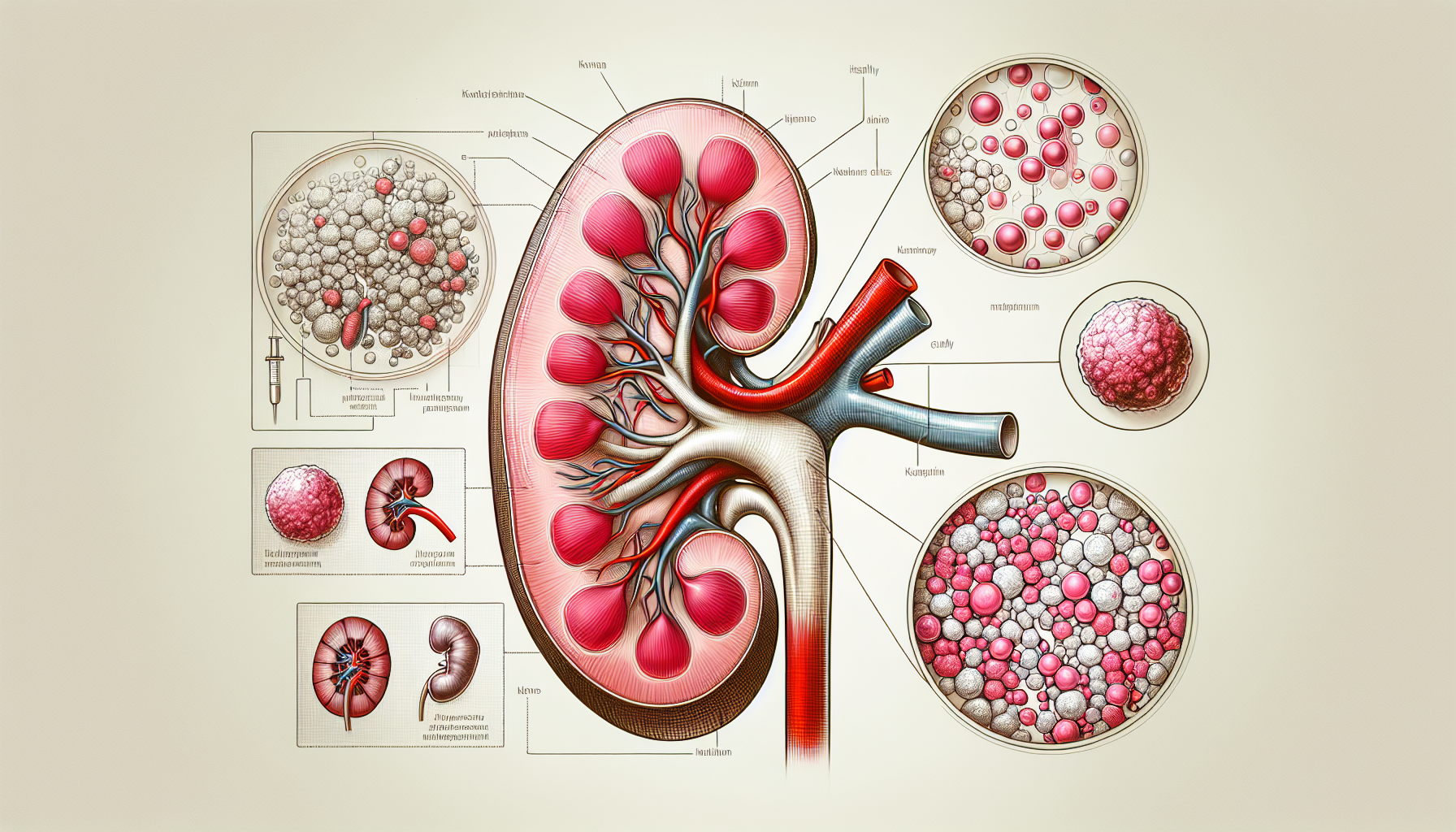
Precision Medicine in Diabetes
In 2018, the American Diabetes Association (ADA), in collaboration with the European Association for the Study of Diabetes (EASD), the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), and the JDRF Diabetes Foundation, launched the Precision Medicine in Diabetes Initiative (PMDI). This initiative focuses on customizing diabetes treatment based on five pillars: diagnostics, prevention, treatment, prognostics, and monitoring.
One significant area of progress is in diagnostics. Thanks to advancements in genomics and environmental studies, it has become easier to identify the specific subtype of diabetes a patient has. This can help doctors choose the most effective therapies based on individual needs.
The Role of Genomics in Tailored Treatment
Genomics, the study of genes and their functions, is playing a key role in this new approach. Genetic data can inform which medications might work best for a particular patient. For example, the same medication could have different effects on two individuals based on their genetic makeup.
This personalized approach could revolutionize how we prescribe diabetes medications, moving away from a 'one-size-fits-all' model to more tailored treatments.
Advancements in Monitoring and AI
Wearable devices and other monitoring tools are also helping to provide more detailed insights into a patient’s daily activities and food intake. This data, combined with genetic information, can be analyzed using artificial intelligence to make more accurate diagnoses and treatment plans.
Lessons from Other Medical Fields
The move to redefine diabetes subtypes is similar to recent changes in other medical fields. One example is the renaming of non-alcoholic fatty liver disease (NAFLD) to metabolic dysfunction-associated steatotic liver disease (MALSD). This change has led to more targeted treatments for the condition.
Similarly, redefining diabetes subtypes could help specialists make better use of the numerous drug classes available for treatment.
The Future of Diabetes Treatment
Currently, there are about a dozen drug classes available for diabetes treatment, but not all of them are equally effective for every patient. Some drugs, like DPP-4 inhibitors, are becoming less popular as we learn more about their limited benefits for certain patients. However, as we gain more genetic data, we might find that some of these drugs are highly effective for specific subtypes.
Artificial intelligence and precision medicine could help re-prioritize these existing drug classes and introduce new ones, making diabetes treatment more effective and personalized.
The Promise of Personalized Care
In summary, the future of diabetes care lies in understanding the unique genetic and environmental factors affecting each patient. This approach could lead to better outcomes and more effective treatments for millions of people living with diabetes.
References
- American Diabetes Associationhttps://diabetes.org
- European Association for the Study of Diabeteshttps://easd.org
- National Institute of Diabetes and Digestive and Kidney Diseaseshttps://www.niddk.nih.gov
- JDRF Diabetes Foundationhttps://www.jdrf.org