Secukinumab Trial Results in Lichen Planus: What You Need to Know
Key Takeaways
- Secukinumab shows promise but did not conclusively prove effectiveness in lichen planus.
- It's generally safe but further trials are needed to confirm its efficacy.
- Different subtypes of lichen planus responded differently to the treatment.
Did You Know?
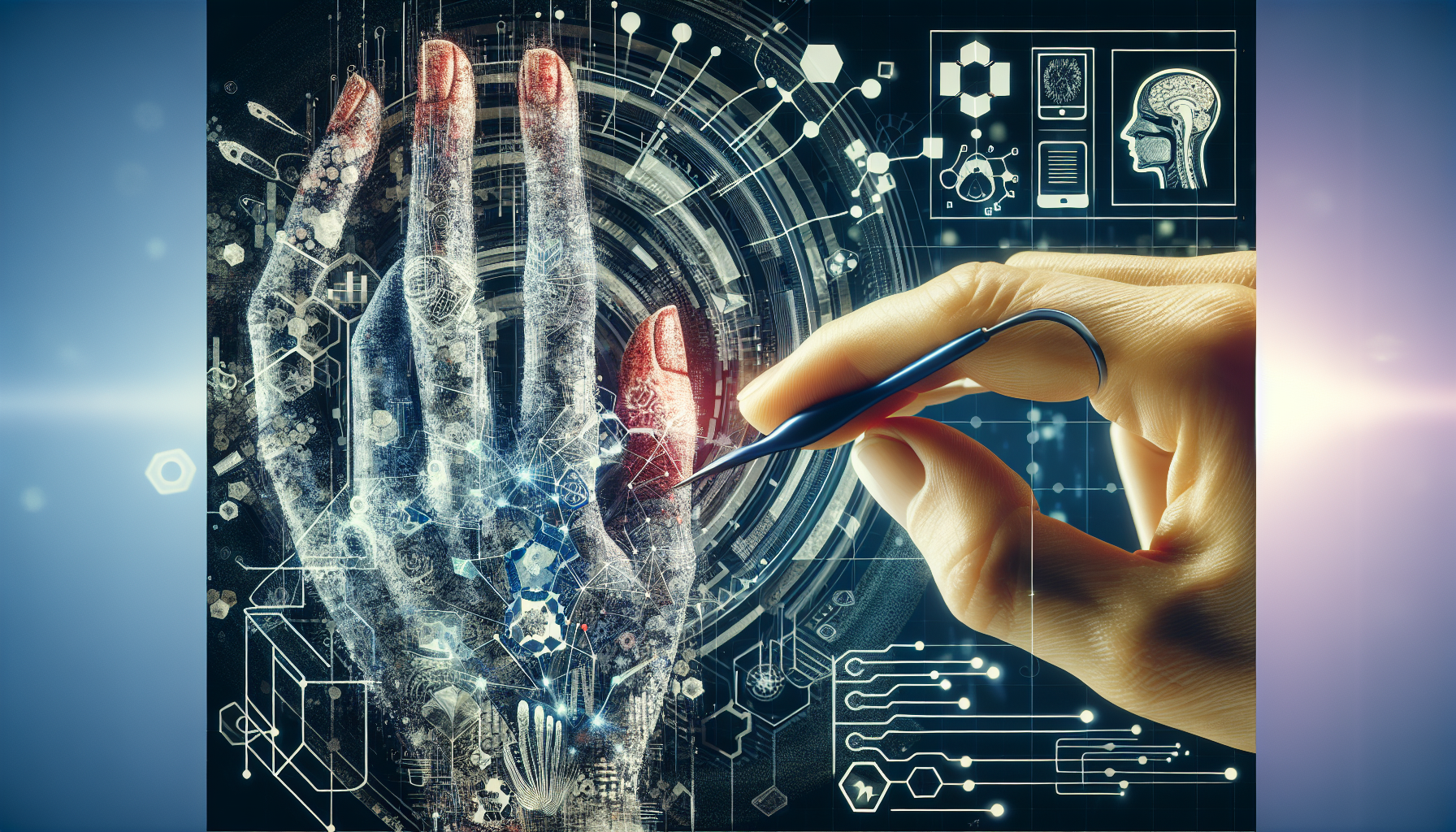
Understanding Lichen Planus
Lichen planus (LP) is a skin condition caused by the immune system attacking the body's own cells. It affects around 1-2% of the population. LP can present in various forms, including cutaneous (skin), mucosae (mouth and genitals), and planopilaris (hair follicles).
Cutaneous lichen planus (CLP) is characterized by severe itching, mucosae lichen planus (MLP) by painful lesions, and lichen planopilaris (LPP) by hair loss. While these symptoms significantly impact patients' quality of life, effective treatments are limited.
The Secukinumab Trial
A trial known as the PRELUDE study aimed to evaluate the effectiveness of secukinumab, an IL-17A inhibitor, in treating various forms of lichen planus. The trial was conducted across multiple centers and included 111 participants divided into three subgroups based on their type of LP.
Participants received 300 mg of secukinumab every 4 weeks for the first 16 weeks, followed by either secukinumab or placebo for another 16 weeks. The main goal was to achieve noticeable clinical improvement by week 16.
Results of the Study
For patients with MLP, 37% of those treated with secukinumab showed at least a 2-grade improvement in disease severity compared to 23.1% in the placebo group. Similarly, those with LPP had a 37.5% improvement rate versus 30.8% with placebo. However, for those with CLP, the placebo group outperformed the secukinumab group (58.3% vs. 44%).
Overall, while MLP and LPP patients showed numerical improvements with secukinumab, the trial did not meet its proof-of-concept criteria, meaning the results weren't strong enough to prove the drug's effectiveness conclusively.
Long-term Outcomes
Patients who had started on secukinumab continued to show improvement through week 32. Those who switched from placebo to secukinumab after 16 weeks also experienced varying degrees of improvement.
Specifically, in the MLP group, 9.1% of those who switched to secukinumab reached a significant improvement by week 32. For LPP patients, the response rate after switching to secukinumab rose to 63.6% by the same period.
Safety and Adverse Events
Overall, secukinumab was well tolerated among the participants. The most common side effects reported included worsening of LP and headaches. One serious adverse event (ulcerative colitis) occurred in the MLP treatment group, leading to treatment discontinuation.
Future Research
The study authors concluded that while secukinumab was safe, further research is needed to confirm its effectiveness, especially in larger trials. The study also raises questions about the role of interleukin-17A in different types of lichen planus, suggesting a need for more robust comparisons of underlying molecular mechanisms.
Conclusion
Secukinumab shows potential but falls short of proving its efficacy in lichen planus, particularly in skin manifestations. It could still be promising for mucosal and follicular forms of the disease.