The Hidden Dangers of Gastrointestinal Bleeding in Advanced CKD
Key Takeaways
- Advanced CKD patients are at a higher risk for GI bleeding.
- Timely endoscopic evaluation is crucial for better health outcomes.
- Ongoing research seeks to improve medical guidelines and patient care.
Did You Know?
Introduction
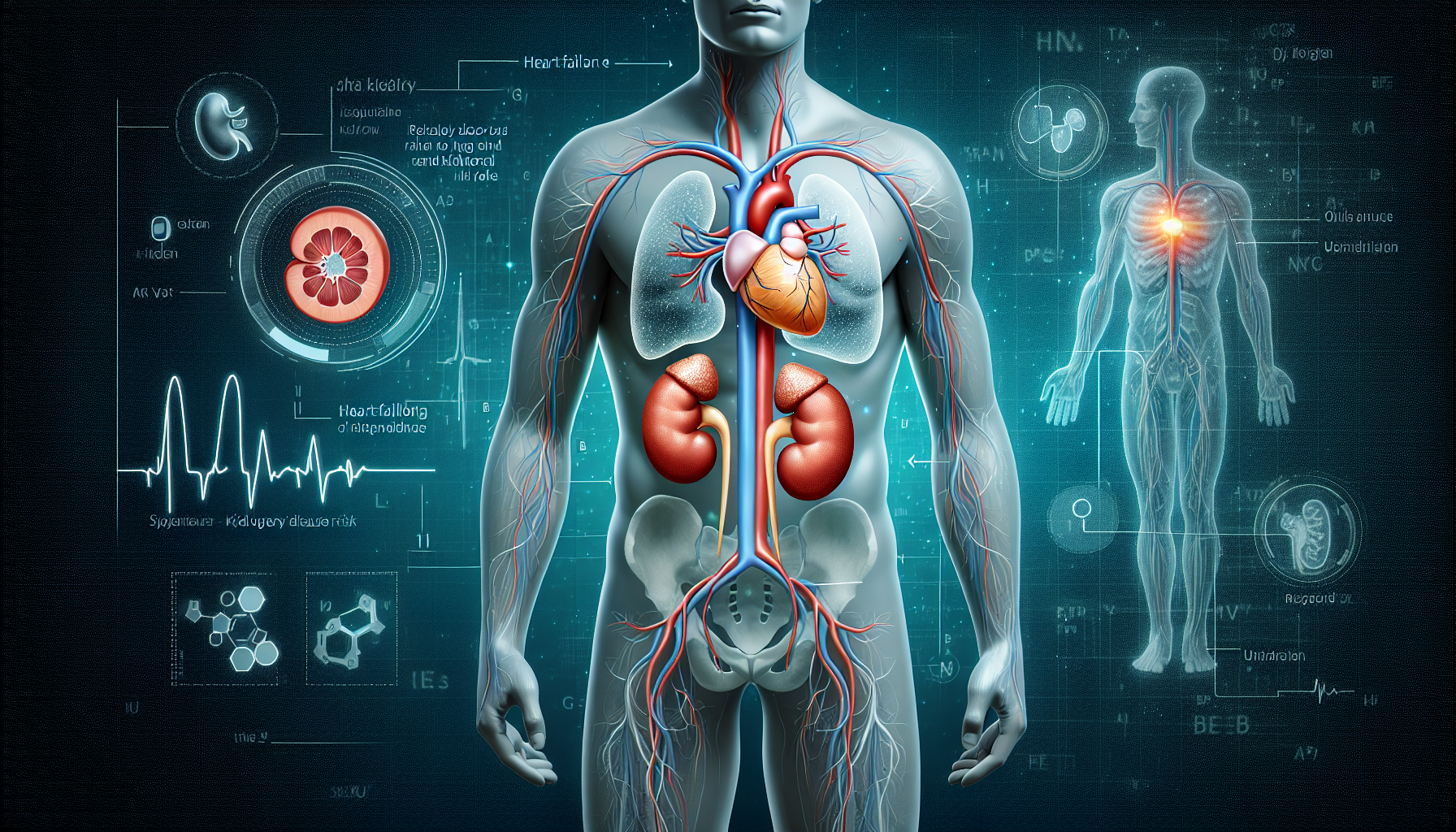
Chronic Kidney Disease (CKD) is a progressive condition that affects millions of people worldwide. When CKD reaches its most advanced stages, patients face numerous health challenges. One of the most alarming issues is the increased risk of gastrointestinal (GI) bleeding, which can be life-threatening.
Increased Risk of GI Bleeding
Recent studies reveal that individuals with stage 5 CKD, the most severe form of the disease, are significantly more likely to experience GI bleeding compared to those without CKD. This risk persists irrespective of whether the patients are on dialysis or not.
Statistics show that stage 5 CKD patients are 40% more likely to be hospitalized due to GI bleeding. This high incidence underscores the need for vigilant medical supervision and timely intervention.
Impact on Hospitalization and Mortality
The consequences of GI bleeding in advanced CKD patients extend beyond hospital admissions. There is a marked increase in inpatient mortality rates among these patients. Stage 5 CKD patients not on dialysis have more than double the odds of all-cause mortality during hospitalization, while those on dialysis face nearly twice the odds.
This elevated mortality risk highlights the critical nature of managing CKD patients with potential GI bleeding, ensuring they receive prompt and effective medical care.
Timing of Endoscopy
Endoscopic evaluation is a key diagnostic and therapeutic tool for GI bleeding. However, patients with stage 5 CKD are less likely to receive early endoscopies, which are crucial for better outcomes. Delayed endoscopies, performed more than 48 hours after admission, significantly raise the chances of mortality.
The reasons for delayed endoscopies include hemodynamic instability, previous endoscopic procedures, and complications related to anesthesia, especially in CKD and end-stage kidney disease (ESKD) patients.
Confounding Factors
Several factors can influence the timing of endoscopic evaluations in CKD patients. Electrolyte imbalances, dialysis schedules, and low platelet counts can lead to delays or cancellations of the procedure. Additionally, the risk of anesthesia-related complications is higher in advanced CKD and ESKD patients, further contributing to the delay.
Research emphasizes the importance of adhering to international guidelines, which recommend endoscopy within 24 hours for acute upper GI bleeding cases. Improved compliance with these guidelines could enhance patient outcomes.
Additional Procedures and Complications
Patients with advanced CKD on dialysis often require additional medical interventions such as angiograms, ventilation support, vasopressor use, and blood transfusions. These procedures increase the complexity and cost of hospital care.
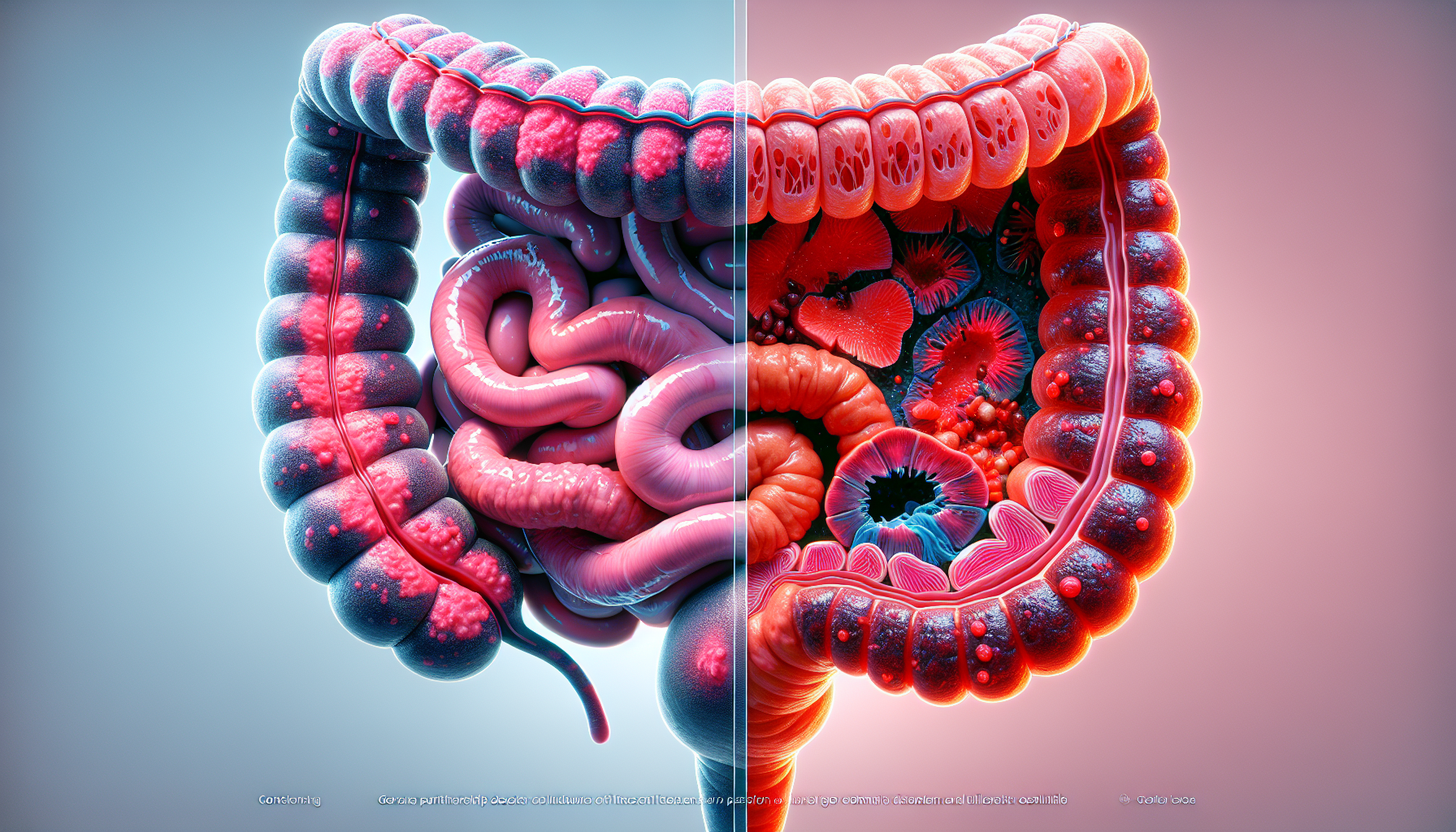
Common causes of GI bleeding in these patients include ulcers and angiodysplasia. Interestingly, the incidence of angiodysplasia appears to decrease following a kidney transplant, highlighting the potential role of uremic factors in platelet dysfunction.
Transplant Patients
For patients who have received a kidney transplant, the risk for certain types of GI bleeding, like diverticular bleeding, remains higher. However, the overall risk of GI bleeding similar to those without CKD, suggesting beneficial effects of transplantation on GI health.
The reduction in angiodysplasia-related bleeding post-transplant could be due to the alleviation of uremic conditions that impair platelet function, pointing to a complex interplay between kidney function and GI health.
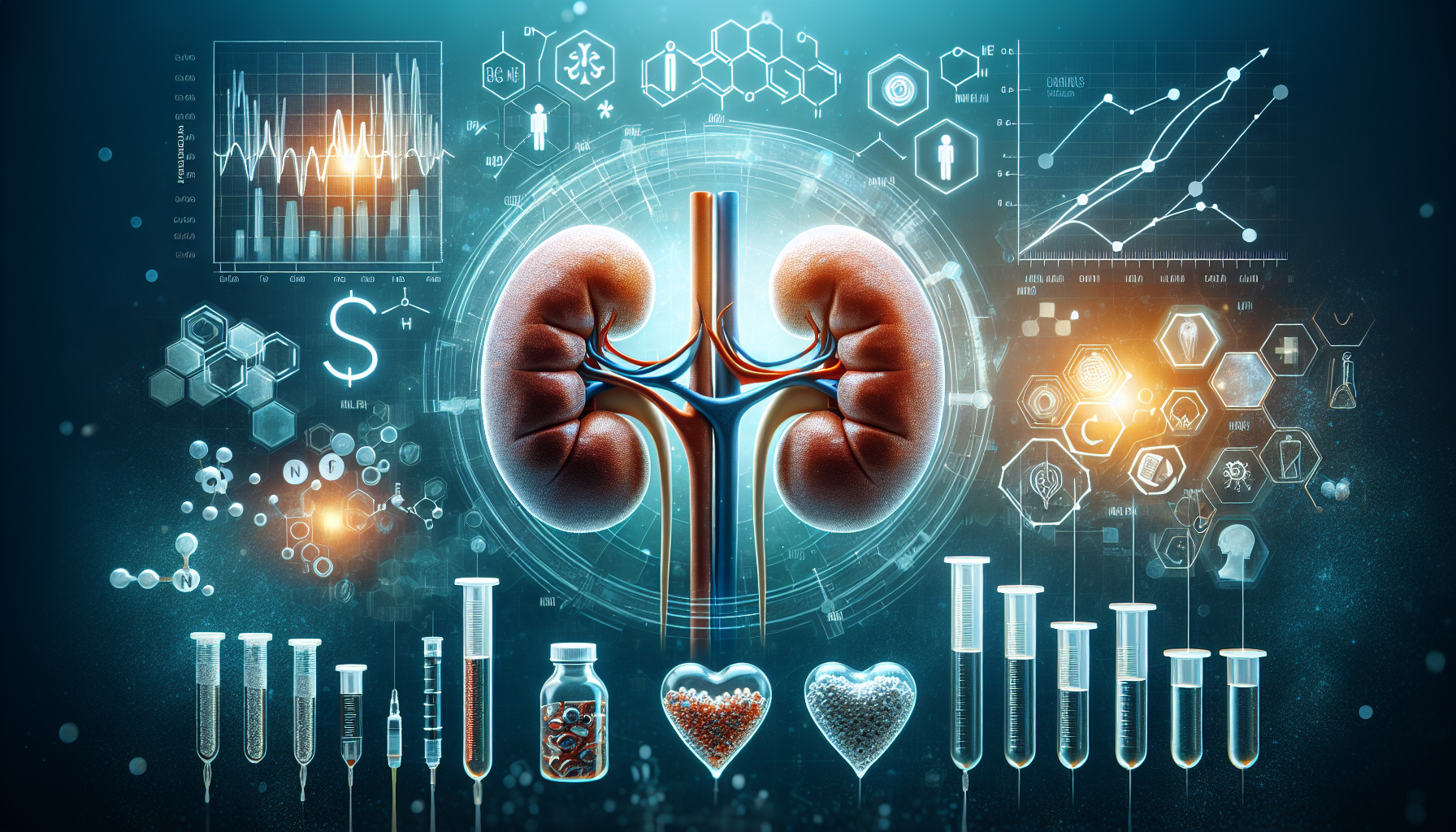
Ongoing Research
The findings discussed are based on data from the 2019 Nationwide Inpatient Sample, encompassing over 500,000 adults admitted with GI bleeding. Further research with expanded sample sizes is planned to better understand these dynamics and improve clinical practices.
Conclusion
Managing advanced CKD presents numerous challenges, with GI bleeding being a significant concern. Timely and effective medical interventions, particularly early endoscopic evaluations, are vital for improving outcomes and reducing mortality in these patients.
Future Implications
Further understanding of the factors influencing delayed endoscopies and developing strategies to mitigate these delays could lead to better adherence to guidelines and improved patient results. Research is ongoing to explore these aspects and enhance the care provided to advanced CKD patients.