Understanding How Sociodemographic Factors Affect Treatment Compliance in Wet AMD
Key Takeaways
- Sociodemographic factors such as insurance coverage, socioeconomic status, marital status, and race significantly influence adherence to wet AMD treatment schedules.
- Challenges such as poverty, limited transportation, and residence in remote areas serve as barriers to consistent treatment access, especially for economically disadvantaged patients.
- Healthcare systems must consider sociodemographic barriers to improve adherence, tailoring services to patient needs through measures like transportation support and flexible scheduling.
Did You Know?
Introduction to Wet AMD and Its Treatment
Wet Age-Related Macular Degeneration (nAMD) is a severe ocular condition that leads to vision loss in individuals, particularly seniors. The primary treatment involves intravitreal injections of anti-VEGF (Vascular Endothelial Growth Factor) medications. These injections are crucial for halting disease progression and improving visual outcomes. However, maintaining strict adherence to treatment schedules is essential for the efficacy of these therapies.
The Impact of Sociodemographic Elements on Treatment Adherence
Recent research indicates that various sociodemographic factors significantly influence the regularity with which patients adhere to their prescribed treatment schedules for nAMD. Factors such as insurance coverage, socioeconomic status, marital status, and race have all been identified as influencing how frequently patients attend their treatment sessions. Patients who are economically disadvantaged or have less stable insurance coverage, for example, often face greater challenges in maintaining consistent treatment adherence.
Challenges Faced by Specific Demographic Groups
Individuals covered by Medicaid or Medicare, as well as those without private insurance, tend to experience longer intervals between treatments. This delay can negatively impact the effectiveness of their management plan for nAMD. Additionally, married individuals generally show slightly better adherence compared to their unmarried counterparts, suggesting the possible role of a support system in managing health appointments.
Barriers to Regular Treatment Visits
Poverty, limited transport options, and residing in remote areas are significant barriers that prevent consistent access to eye care facilities. These issues are more pronounced in lower socioeconomic groups, who might also struggle with the direct costs related to treatment.
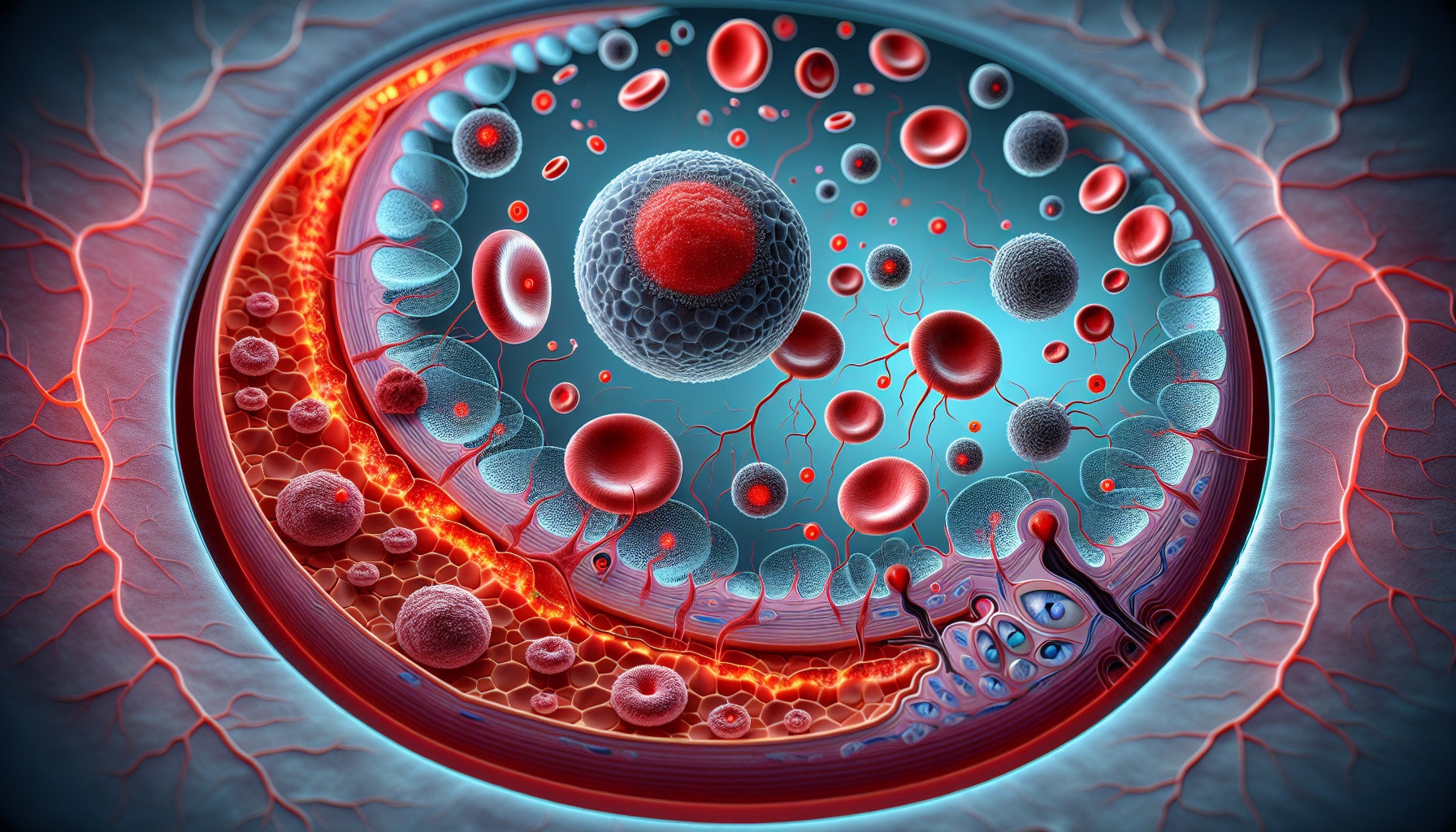
Effect of Patient Adherence on Visual Health
Skipping treatments or irregularly adhering to the treatment schedule can lead to a marked decline in visual acuity. Continuous and timely treatment is crucial to prevent worsening of the condition, highlighting the importance of addressing the barriers faced by different demographic groups.
Role of Healthcare Systems and Providers
Healthcare systems and providers play a critical role in accommodating the diverse needs of patients. Understanding the sociodemographic barriers can help healthcare providers to tailor their services to improve adherence, such as by offering transportation services or more flexible scheduling options.
Insights from Recent Studies and Future Outlook
A retrospective study led by Alison Choi at the University of Pittsburgh analyzed adherence patterns among over 900 nAMD patients. This study underlines the significance of considering sociodemographic factors when designing interventions to improve patient outcomes in eye care. The insights derived help in strategizing more inclusive and effective healthcare provisions that can lead to better management of wet AMD.