Understanding Surgical Treatment for Bone Infections in Children
Key Takeaways
- Pediatric osteomyelitis is a bone infection that often needs antibiotics and sometimes surgery.
- Diagnostic imaging like MRIs are essential for accurate treatment planning.
- Post-surgery care and long-term follow-up are crucial for successful recovery.
Did You Know?
What is Pediatric Osteomyelitis?
Pediatric osteomyelitis is an infection that affects the bones in children. This condition is quite common and has been on the rise over the years. It can be caused by bacteria such as Staphylococcus aureus, streptococci, and H. influenzae type B. The rate of this infection can range from 8 to 10 per 100,000 children in wealthy countries, to 80 per 100,000 in poorer countries.
Initial Treatment Approaches
The first step in treating pediatric osteomyelitis usually involves antibiotic therapy. These medications aim to eliminate the bacteria causing the infection. However, if the antibiotics do not work or if the child develops an abscess, surgery might be necessary.
When is Surgery Needed?
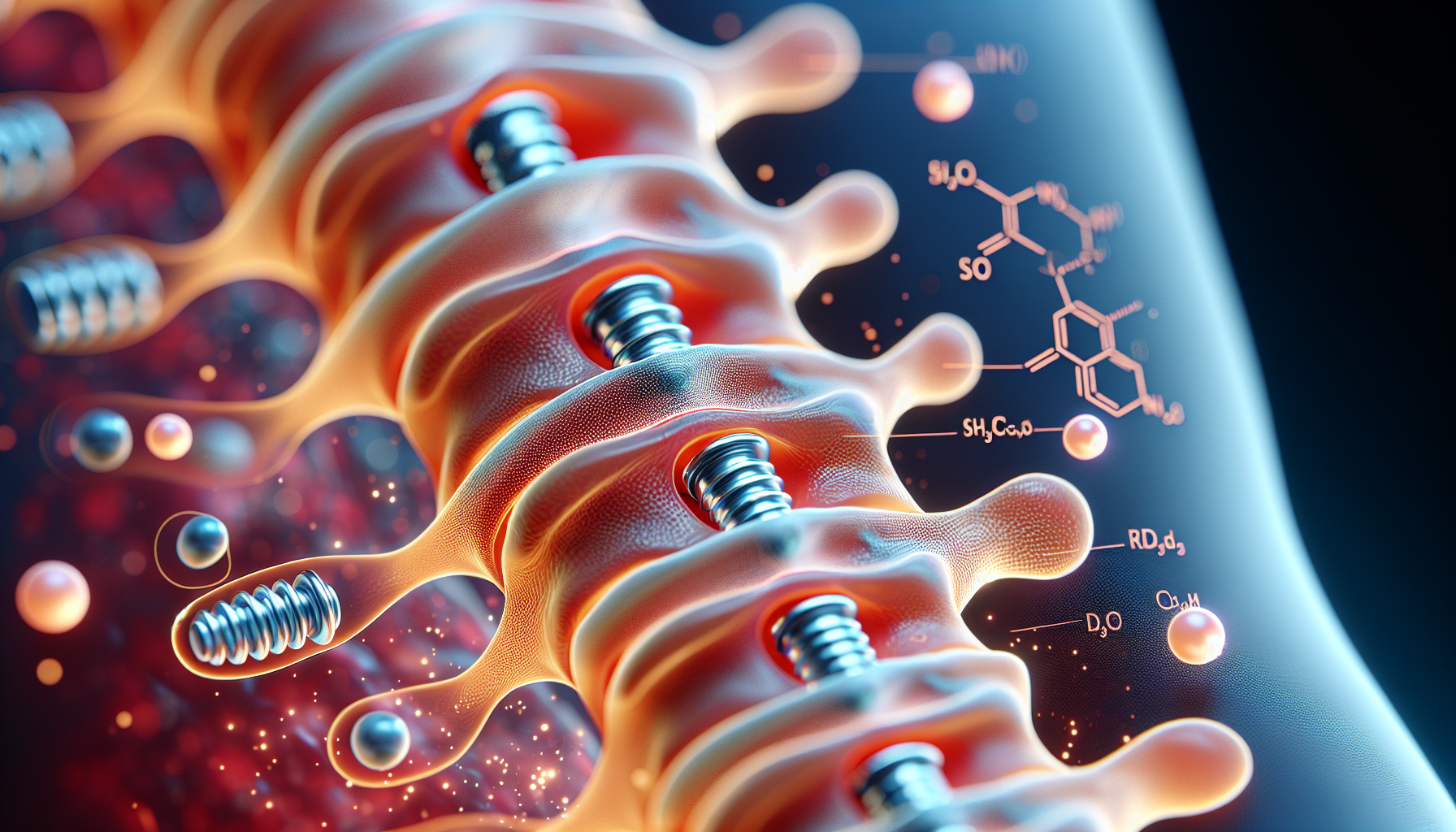
Surgical debridement is considered when the initial antibiotic therapy fails or in more severe cases of osteomyelitis. Certain clues that indicate a need for surgery include an infection that doesn’t respond to antibiotics, evidence of dead bone, or the presence of an abscess or deep fluid collections. Various other indicators might necessitate surgery as well, like infected joints or prosthetic material.
Risks and Benefits of Surgical Debridement
Although surgery comes with some risks such as bone death, fractures, or growth problems, it also offers significant benefits. Combining surgical debridement with proper antibiotic treatment can lead to good clinical outcomes and improved functionality for the child.
Diagnosis and Planning for Surgery
Diagnosing osteomyelitis involves taking the child’s medical history and conducting a physical exam. Doctors look for signs like cellulitis, tenderness, or sinus tracts that indicate infection spread. Imaging techniques like radiographs and MRIs help pinpoint the infection’s location and extent.
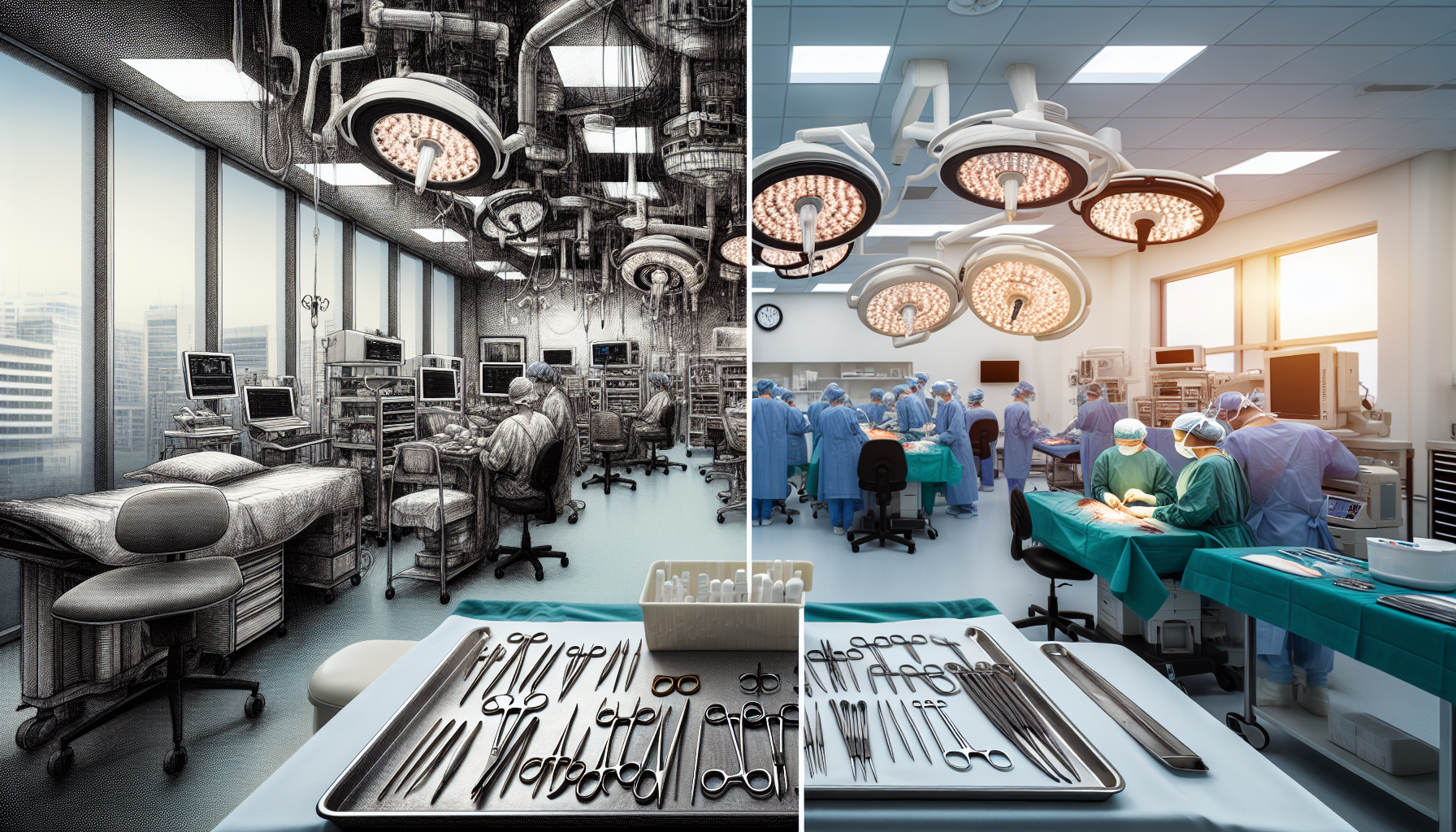
Surgical Procedure for Osteomyelitis
During surgery, the child is usually put under general anesthesia. Surgeons take steps to locate and access the infected area, often using imaging tools to guide them. They carefully remove the infected tissue and fluid and send samples for lab tests to identify the causative bacteria.
Post-Surgery Care
Post-operative care involves thorough irrigation of the surgical site, using a large volume of sterile fluid to clean out the infection. The site is then closed in layers to minimize dead space and reduce the risk of new infections. Drains are placed to allow any remaining infected fluid to escape, which can be removed once the output decreases.
Recovery and Follow-Up
After surgery, the child’s recovery is closely monitored. Regular lab tests check for decreases in infection markers. If necessary, additional MRIs may be performed to identify any persisting infection areas. The child is usually seen for follow-up visits within 10 to 14 days after surgery and continues under the care of infectious disease specialists while on antibiotics.
Long-Term Follow-Up
For children whose infections affected critical areas of the bone, such as growth plates, long-term follow-up is essential. This ensures monitoring for any possible growth issues or deformities due to the infection or surgery.
Important Considerations for Parents
Being aware of the infection signs and understanding the treatment process is crucial for parents. Early recognition and proper medical intervention can significantly improve the outcome for children with osteomyelitis.