Understanding the Link Between Rheumatoid Arthritis and Depression
Key Takeaways
- RA patients often experience major depressive disorder.
- Severity of RA correlates with psychiatric conditions.
- Integrated care approaches improve patient outcomes.
Did You Know?
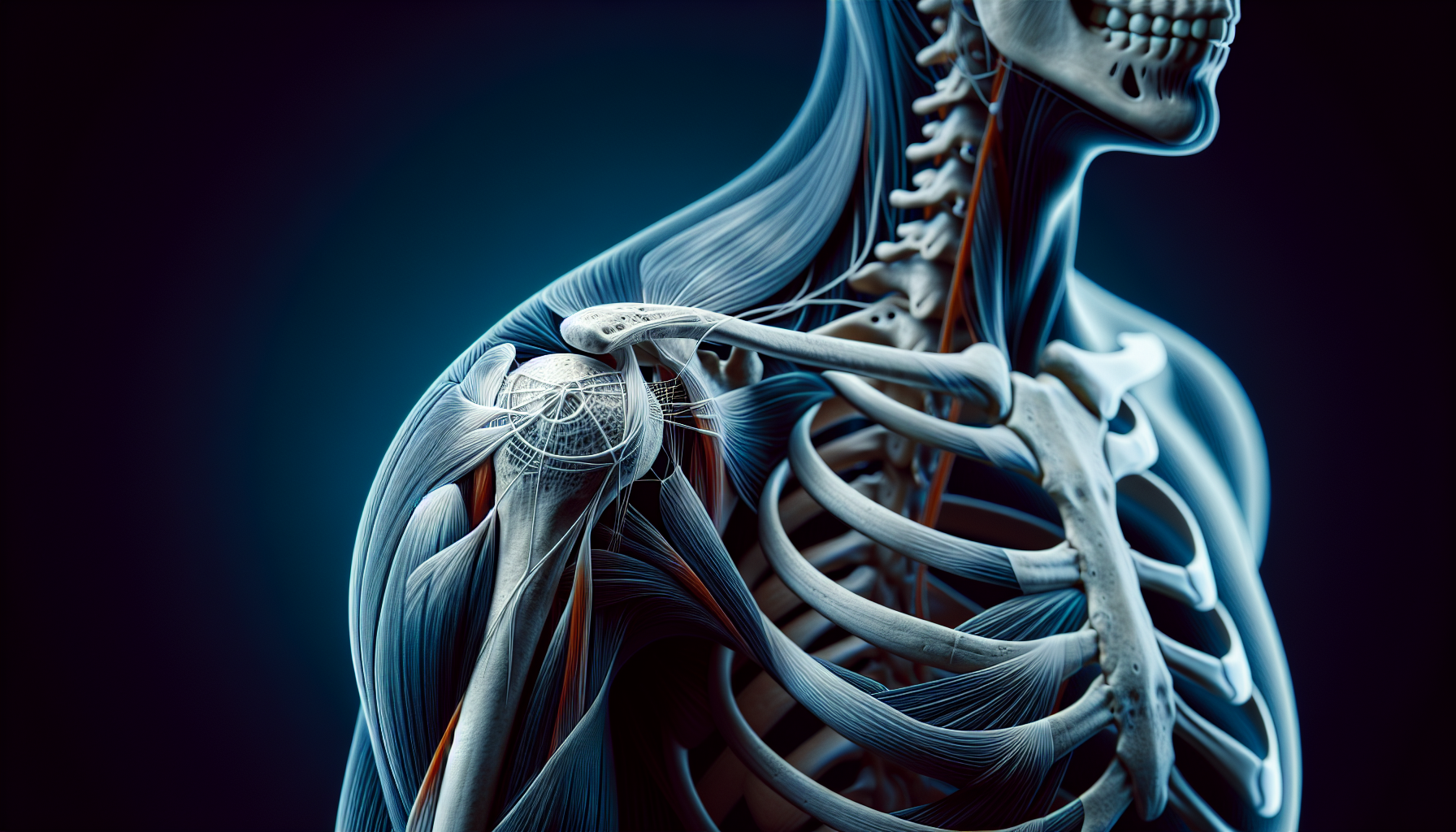
Introduction to Rheumatoid Arthritis and Mental Health
Rheumatoid Arthritis (RA) is a chronic condition characterized by inflammation and pain in the joints. While it primarily affects physical health, RA also takes a significant toll on mental well-being. Recent research highlights the prevalence of psychiatric comorbidities such as major depressive disorder (MDD) in patients suffering from RA.
Prevalence of Psychiatric Conditions in RA Patients
A recent study discovered that MDD is the most common psychiatric condition observed in patients with RA, with an alarming incidence rate. The study also noted the prevalence of other mental health issues like somatoform disorders and generalized anxiety disorder (GAD).
Among the 1000 patients studied, nearly 80% experienced some form of psychological distress, with MDD leading the list.
Factors Contributing to Mental Health Issues in RA
Various factors contribute to the high rates of mental health conditions in RA patients. Chronic pain, persistent inflammation, and the ongoing burden of managing a long-term illness can significantly affect a patient's emotional well-being. Additionally, medication side effects and the societal impact of being diagnosed with a chronic condition further exacerbate mental health issues.
The Study's Methodology
The research was conducted over three years at Shifa Hospital and V Care Super Specialty Clinic in Srinagar, India. Patients were assessed using the International Classification of Diseases-10 (ICD-10) criteria and the Mini-International Neuropsychiatric Interview Schedule PLUS.
The study included a diverse range of patients aged 17 years and older, with a substantial portion being female. The Disease Activity Score with a 28-joint count was used to measure the severity of the rheumatoid arthritis in each patient.
Age and Gender Differences in Mental Health
The study found significant age and gender differences in the prevalence of MDD among RA patients. Younger patients (<55 years) had a higher prevalence of MDD compared to older patients. Additionally, females were more likely to experience MDD and other psychiatric conditions compared to their male counterparts.
Impact of Disease Severity on Mental Health
There was a direct correlation between the severity of RA and the prevalence of MDD. Patients with high disease activity had a higher incidence of depression compared to those with moderate or low disease activity. This highlights the need for comprehensive treatment that addresses both physical and mental health aspects in RA patients.
Study Limitations and Areas for Future Research
The investigators pointed out some limitations in their study, such as the inability to generalize the results to the broader Indian population and not recording management strategies for the identified psychiatric morbidities. There is also a potential for recall bias.
Despite these limitations, the study provides valuable insights into the psychiatric comorbidities associated with RA and emphasizes the need for integrated care approaches.
Importance of Integrated Care
Given the high rates of psychiatric morbidity among RA patients, there is a crucial need for integrated care models that include both rheumatologic and psychiatric services. Early detection and management of mental health issues can significantly improve treatment outcomes and overall quality of life for RA patients.
Conclusion
This study underscores the significant overlap between RA and various psychiatric conditions, particularly MDD. Healthcare providers should be aware of these risks and incorporate mental health assessments into routine care for RA patients.
Future Directions
Future research should focus on broader population samples and explore effective management strategies for both RA and its associated psychiatric conditions. A holistic approach is essential for optimal patient outcomes and quality of life.
References
- Arthritis Foundationhttps://www.arthritis.org
- American College of Rheumatologyhttps://www.rheumatology.org
- National Institute of Mental Healthhttps://www.nimh.nih.gov