Breakthrough in Heart Disease: Aficamten Shows Promising Results for HCM Patients
Key Takeaways
- Aficamten, a cardiac myosin inhibitor, has significantly improved exercise capacity and quality of life for obstructive hypertrophic cardiomyopathy (HCM) patients in a recent SEQUOIA-HCM trial.
- The safety profile of Aficamten closely matches that of a placebo and shows fewer incidences of systolic dysfunction compared to other cardiac myosin inhibitors, making it a promising option for HCM treatment.
- If approved by the FDA, Aficamten could dramatically change current HCM treatment paradigms, potentially reducing the need for invasive procedures and offering faster symptom relief.
Did You Know?
Introduction to Aficamten and its Impact on Obstructive HCM
Aficamten, a cardiac myosin inhibitor, is currently illuminating paths in the treatment of obstructive hypertrophic cardiomyopathy (HCM), potentially altering the landscape of heart disease management. A study detailed in the SEQUOIA-HCM trial has demonstrated significant advancements in both the exercise capacity and overall quality of life for those afflicted with obstructive HCM.
By specifically targeting the cardiac muscle's proteins, Aficamten helps reduce the heart's struggle against obstructive flows, thereby increasing oxygen uptake which is a central factor in the physical capabilities and well-being of these patients.
Study Findings and Clinical Data
The landmark study enrolled 282 participants who were already undergoing standard treatments for obstructive HCM. The revealing outcomes of Aficamten versus a placebo shed light on not only enhanced physical function but also notable improvements in daily living and cardiac health over a 24-week period.
Results showcased that Aficamten-treated patients experienced a pivotal increase in peak oxygen uptake (VO2 max), which is directly linked to a decreased risk of severe outcomes like heart failure or the need for transplantation.
Moreover, improvement trends extended beyond physical metrics, positively affecting subjective health statuses measured by the Kansas City Cardiomyopathy Questionnaire (KCCQ), instigating a broader perspective on patient well-being.
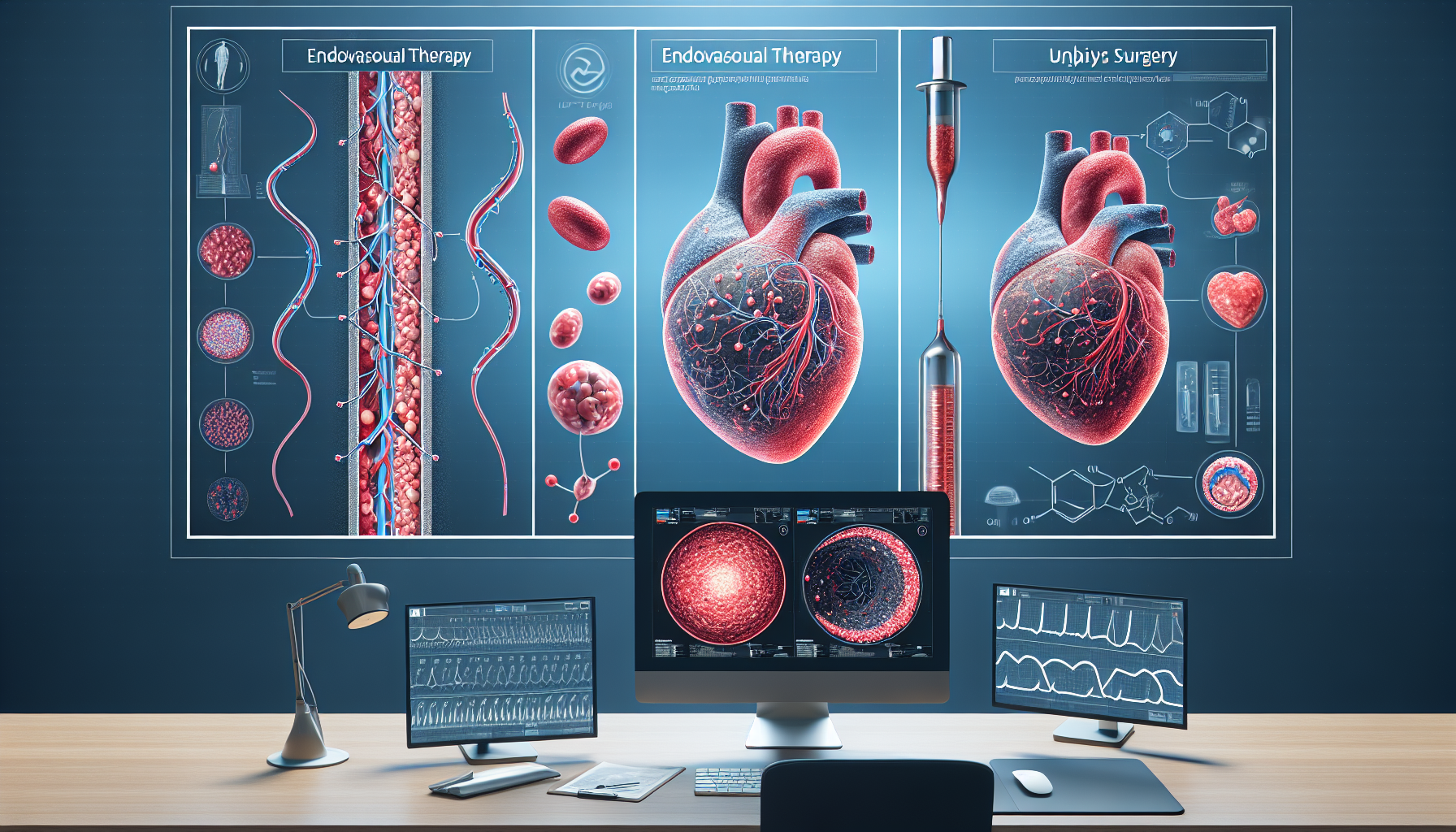
Comparative Safety and Efficacy
The safety profile of Aficamten aligned closely with that of the placebo group, reassuring its use in clinical settings. This aligns with the therapeutic goal of minimizing adverse effects while maximizing treatment benefits. Additionally, notable differences between Aficamten and other cardiac myosin inhibitors present in its low incidences of systolic dysfunction, a common side effect in this drug category.
Implications for HCM Treatment
Should Aficamten gain FDA approval, it would mark a significant milestone as the second cardiac myosin inhibitor in the U.S. marketplace. This approval could potentially shift current treatment paradigms, offering a more effective and rapid relief for HCM symptoms compared to the existing therapies.
By lessening physical restrictions and improving heart functionality, Aficamten might reduce the number of days patients are eligible for more invasive treatments like septal reduction therapy, which is often a last resort.
Final Thoughts and Future Directions
While further research is required to fully validate Aficamten's long-term benefits and its role within broader therapeutic protocols, the evidence thus far propels this treatment forward as a considerable option for improving life quality in HCM patients. The heart community closely watches as this drug progresses through regulatory phases and towards potential widespread clinical use.