Exploring the Connection Between Asthma and Heart Disease
Key Takeaways
- Asthma's Type 2 inflammation is linked to higher heart disease risk.
- Elevated eosinophil counts are associated with increased CAD risk.
- Comprehensive care is essential to manage both asthma and heart health.
Did You Know?
Understanding Asthma and Its Inflammatory Impact
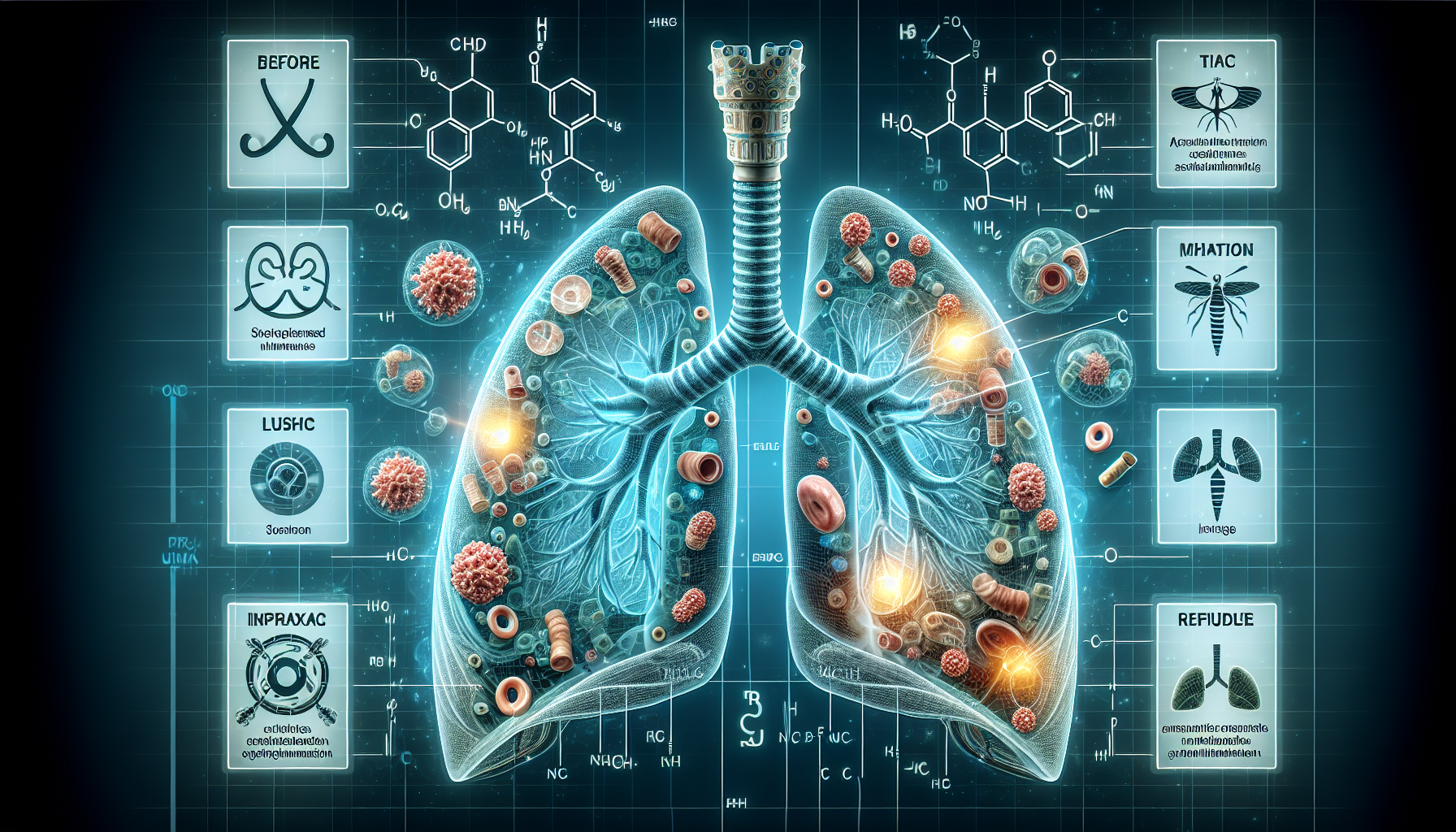
Asthma is a chronic respiratory condition that is characterized by inflammation of the airways, leading to symptoms like wheezing, shortness of breath, and coughing. While it is well-established that asthma impacts respiratory health, recent research has unveiled a concerning link between asthma and coronary artery disease (CAD), a condition marked by the narrowing or blockage of coronary arteries.
The inflammation associated with asthma, particularly Type 2 inflammation, is now being scrutinized for its role in increasing the risk of heart disease. Type 2 inflammation involves elevated levels of certain immune cells such as eosinophils, which can also be triggered by allergies and other inflammatory conditions.
The Study: A Deeper Dive into the Asthma-Heart Disease Link
A team of researchers, led by Dr. Christa McPhee from the Icahn School of Medicine at Mount Sinai, presented findings at the American Thoracic Society International Conference that emphasize this connection. The study utilized data from over 11,000 adults in the UK Biobank, focusing on those who follow the Global Initiative for Asthma treatment guidelines and exhibit signs of Type 2 inflammation.
Participants with underlying pulmonary conditions such as COPD, bronchiectasis, and interstitial lung disease were excluded to refine the study's focus. The investigation accounted for various factors like BMI and cholesterol levels to isolate the impact of asthma and Type 2 inflammation on CAD risk.
Key Findings: Eosinophils and Heart Disease
One of the notable discoveries was the significant correlation between higher eosinophil counts and increased risk for coronary artery disease. Eosinophils, a type of white blood cell, are often elevated in individuals with asthma and other allergic conditions.
The data revealed that patients with higher eosinophil counts had a notably higher likelihood of developing CAD, even when other risk factors were controlled. This highlights the importance of monitoring inflammatory markers in asthma patients to better manage and mitigate cardiovascular risks.
Implications for Asthma Management
Given these findings, healthcare providers are encouraged to recognize the cardiovascular implications of chronic asthma. Evidence of high Type 2 inflammation should be considered a red flag for potential heart disease risk, necessitating a comprehensive treatment approach that addresses both respiratory and cardiovascular health.
This insight also underscores the need for specialized asthma care, potentially involving referrals to pulmonologists for optimized management of airway inflammation.
The Road Ahead: Future Research Directions
While the current study provides valuable insights, it also opens up avenues for future research. Investigations into specific asthma medications, particularly biologics, could shed light on their protective effects against cardiovascular diseases.
Prospective studies aimed at understanding the long-term impacts of asthma and Type 2 inflammation on heart health will be essential. Additionally, examining the intricate dynamics between various inflammatory markers and cardiovascular outcomes could lead to more targeted therapies.
Conclusion
The link between asthma, Type 2 inflammation, and coronary artery disease highlights a critical intersection of respiratory and cardiovascular health. By continuing to explore these connections, the medical community can develop better strategies for managing asthma and preventing its potential cardiovascular complications.
References
- American Thoracic Societyhttps://www.thoracic.org/
- UK Biobankhttps://www.ukbiobank.ac.uk/
- Icahn School of Medicine at Mount Sinaihttps://icahn.mssm.edu/